Abstract
OBJECTIVE: Prior studies have shown that 60% to 75% of adults with upper respiratory tract infections want antibiotics. More recent research indicates declines in antibiotic prescribing for upper respiratory tract infections. To investigate whether there has been a comparable decrease in patients’ desire for antibiotics, we measured the proportion of adults with upper respiratory tract infections who wanted antibiotics in the winter of 2001–2002. We also sought to identify factors independently associated with wanting antibiotics and antibiotic prescribing.
DESIGN: Prospective survey of adults with upper respiratory tract infections prior to visiting an acute care clinic from November 2001 to February 2002.
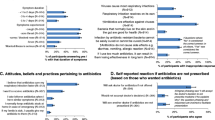
MEASUREMENTS AND MAIN RESULTS: Thirty-nine percent of 310 patients wanted antibiotics. Many patients wanted relief from symptoms (43%) or pain (24%) and many patients expected to receive a diagnosis (49%) or reassurance during the visit (13%). In multivariable modeling, independent predictors of wanting antibiotics were prior antibiotic use (odds ratio [OR], 2.4; 95% confidence interval [CI], 1.3 to 4.7) and current smoking (OR, 3.1; 95% CI, 1.3 to 7.3). Physicians prescribed antibiotics to 46% of patients who wanted antibiotics and 29% of patients who did not want antibiotics (P=.01). In multivariable modeling, wanting antibiotics was an independent predictor of antibiotic prescribing (OR, 2.1; 95% CI, 1.1 to 4.4).
CONCLUSIONS: Only 39% of adults seeking care for upper respiratory tract infections wanted antibiotics, less than in previous studies. In continuing efforts to break the cycle of inappropriate antibiotic use, physicians should not assume that most patients with upper respiratory tract infections want antibiotics.
Similar content being viewed by others
References
Cherry DK, Burt CW, Woodwell DA. National Ambulatory Medical Care Survey: 1999 Summary Advance Data from Vital and Health Statistics No 322. Hyattsville, Md: National Center for Health Statistics; 2001.
Hughes JM, McCaig LF. Trends in antimicrobial prescribing rates for children and adolescents. JAMA. 1995;273:214–9.
Mainous AG, III, Hueston WJ, Clark JR. Antibiotics and upper respiratory infection: do some folks think there is a cure for the common cold. J Fam Prac. 1996;42:357–61.
Gonzales R, Steiner JF, Sande MA. Antibiotic prescribing for adults with colds, upper respiratory tract infections, and bronchitis by ambulatory care physicians. JAMA. 1997;278:901–4.
Nyquist AC, Gonzales R, Steiner JF, Sande MA. Antibiotic prescribing for children with colds, upper respiratory tract infections, and bronchitis. JAMA. 1998;279:875–7.
Metlay JP, Stafford RS, Singer DE. National trends in the use of antibiotics by primary care physicians for adult patients with cough. Arch Intern Med. 1998;158:1813–8.
Hirschmann JV. Antibiotics for common respiratory tract infections in adults. Arch Intern Med. 2002;162:256–64.
Seppala H, Klaukka T, Vuopio-Varkila J, et al. The effect of changes in the consumption of macrolide antibiotics on erythromycin resistance in group A streptococci in Finland. Finnish Study Group for Antimicrobial Resistance. N Engl J Med. 1997;337:441–6.
Butler CC, Rollnick S, Pill R, Maggs-Rapport F, Stott N. Understanding the culture of prescribing: qualitative study of general practitioners’ and patients’ perceptions of antibiotics for sore throats. BMJ. 1998;317:637–42.
Vinson DC, Lutz LJ. The effect of parental expectations on treatment of children with a cough: a report from ASPN. J Fam Prac. 1993;37:23–7.
Macfarlane J, Holmes W, Macfarlane R, Britten N. Influence of patients’ expectations on antibiotic management of acute lower respiratory tract illness in general practice: questionnaire study. BMJ. 1997;315:1211–4.
Hamm RM, Hicks RJ, Bemben DA. Antibiotics and respiratory infections: are patients more satisfied when expectations are met? J Fam Prac. 1996;43:56–62.
Dosh SA, Hickner JM, Mainous AG, III, Ebel MH. Predictors of antibiotic prescribing for nonspecific upper respiratory infections, acute bronchitis, and acute sinusitis. An UPRNet study. Upper Peninsula Research Network. J Fam Prac. 2000;49:407–14.
Ray DA, Rohren CH. Characteristics of patients with upper respiratory tract infection presenting to a walk-in clinic. Mayo Clinic Proc. 2001;76:169–73.
Finkelstein JA, Davis RL, Dowell SF, et al. Reducing antibiotic use in children: a randomized trial in 12 practices. Pediatrics. 2001;108:1–7.
Linder JA, Stafford RS. Antibiotic treatment of adults with sor e throat by community primary care physicians: a national survey 1989–99. JAMA. 2001;286:1181–6.
McCaig LF, Besser RE, Hughes JM. Trends in antimicrobial prescribing rates for children and adolescents. JAMA. 2002;287:3096–102.
Little P, Williamson I, Warner G, Gould C, Gantley M, Kinmonth AL. Open randomised trial of prescribing strategies in managing sore throat. BMJ. 1997;314:722–7.
Hong JS, Philbrick JT, Schorling JB. Treatment of upper respiratory infections: do patients really want antibiotics? Am J Med. 1999;107:511–5.
Sanchez-Menegay C, Hudes ES, Cummings SR. Patient expectations and satisfaction with medical care for upper respiratory infections. J Gen Intern Med. 1992;7:432–4.
Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42:121–30.
Gonzales R, Bartlett JG, Besser RE, et al. Principles of appropriate antibiotic use for treatment of acute respiratory tract infections in adults: background, specific aims, and methods. Ann Intern Med. 2001;134:479–86.
Scott JG. Antibiotic use in acute respiratory infections and the ways patients pressure physicians for a prescription. J Fam Prac. 2001;50:853–8.
Author information
Authors and Affiliations
Corresponding author
Additional information
Funding sources: Dr. Linder was supported in part by National Research Service Award 5T32PE11001-12.
Rights and permissions
About this article
Cite this article
Linder, J.A., Singer, D.E. Desire for antibiotics and antibiotic prescribing for adults with upper respiratory tract infections. J GEN INTERN MED 18, 795–801 (2003). https://doi.org/10.1046/j.1525-1497.2003.21101.x
Issue Date:
DOI: https://doi.org/10.1046/j.1525-1497.2003.21101.x