Abstract
Infection by the new corona virus strain SARS-CoV-2 and its related syndrome COVID-19 has been associated with more than two million deaths worldwide. Patients of higher age and with preexisting chronic health conditions are at an increased risk of fatal disease outcome. However, detailed information on causes of death and the contribution of pre-existing health conditions to death yet is missing, which can be reliably established by autopsy only. We performed full body autopsies on 26 patients that had died after SARS-CoV-2 infection and COVID-19 at the Charité University Hospital Berlin, Germany, or at associated teaching hospitals. We systematically evaluated causes of death and pre-existing health conditions. Additionally, clinical records and death certificates were evaluated. We report findings on causes of death and comorbidities of 26 decedents that had clinically presented with severe COVID-19. We found that septic shock and multi organ failure was the most common immediate cause of death, often due to suppurative pulmonary infection. Respiratory failure due to diffuse alveolar damage presented as immediate cause of death in fewer cases. Several comorbidities, such as hypertension, ischemic heart disease, and obesity were present in the vast majority of patients. Our findings reveal that causes of death were directly related to COVID-19 in the majority of decedents, while they appear not to be an immediate result of preexisting health conditions and comorbidities. We therefore suggest that the majority of patients had died of COVID-19 with only contributory implications of preexisting health conditions to the mechanism of death.
Similar content being viewed by others
Introduction
More than 100 million confirmed cases of coronavirus disease 2019 (COVID-19) and more than two million associated deaths have been counted around the globe by end-January, 20211. COVID-19 is caused by infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), a novel and highly contagious coronavirus strain that mostly spreads through respiratory droplets and that has first been identified in Wuhan, China2.
Some SARS-CoV-2 infections are asymptomatic while most cause mild to moderate illness with respiratory and flu-like symptoms, including fever, chills, cough and sore throat3,4. However, a significant number of patients with COVID-19 develops critical illness and requires intensive care with mechanical ventilation or extracorporeal membrane oxygenation5,6. Especially in these cases, the disease may ultimately be fatal7. While raw numbers of deaths suggest overall COVID-19 case-fatality rates of more than 5%1, infection-fatality rates probably are lower and may range around 0.3–0.5%8.
The risk of death from COVID-19 strongly depends on age and previous health conditions. Older patients and those with chronic comorbidities, such as cardiovascular disease, hypertension, diabetes, and pulmonary disease, are much more prone to critical and fatal disease outcomes4,9. These associations may contribute to an uncertainty to what extent COVID-19 or preexisting health conditions determined the time of a patient’s death. Detailed information on the causality and mechanism of death, as well as the spectrum of comorbidities in cases with fatal outcome that will allow accurate assessment of the hazardous nature of COVID-19 yet is missing.
Autopsies are the gold standard for the analysis of medical conditions and causes of death. Few reports described damage to several organs due to COVID-19 on the morphological level. However, while one study reported fatal pulmonary thromboembolism in few cases10, systematic information on immediate and underlying causes of death are scarce. Here, we present data on clinical and autoptic causes of death and comorbidities of 26 patients that had died after SARS-CoV-2 infection and COVID-19 in Berlin, Germany. Our findings reveal that causes of death were directly related to COVID-19 in most cases and not an immediate consequence of preexisting health conditions and comorbidities, i.e. these patients—despite often suffering from severe health conditions—would not have died in the absence of a SARS-CoV-2 infection at the given time point.
Methods
Study design and clinical information
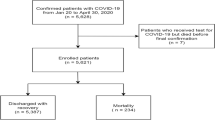
We prospectively included all 26 autopsy cases of hospitalized patients that had died between 1st of March and 19th of June 2020. All patients had been treated for COVID-19 at either Charité—Universitätsmedizin Berlin (n = 22), or an affiliated teaching hospital including Immanuel Klinikum Bernau (n = 1), Vivantes Hospitals Berlin (n = 1), DRK Kliniken Berlin (n = 1), and Klinikum Ernst von Bergmann (n = 1). In all cases, SARS-CoV-2 infection was confirmed by PCR testing of material from nasal and pharyngeal swabs. Informed consent was given by the next of kin, and autopsies were performed on the legal basis of §1 SRegG BE of the autopsy act of Berlin and §25(4) of the German Infection Protection Act. This study was approved by the Ethics Committee of the Charité (EA1/144/13 and EA2/066/20) as well as by the Charité-BIH COVID-19 research board and was in compliance with the Declaration of Helsinki.
Clinical information on comorbidities, pre-existing conditions, microbiological test results and medical management was obtained from patient files and clinical death certificates. Sepsis and septic shock were clinically defined according to the current consensus of Sepsis-311. Cause of death statements were structured in analogy to the guidelines of the World Health Organization (WHO) into immediate causes of death, conditions leading to cause of death, underlying cause, and further relevant conditions that may have contributed to fatal outcome12. Briefly, the immediate cause of death represented the condition (disease, injury or complication) that preceded death most directly. The condition leading to the cause of death indicated a sequence with an etiological or pathological basis that prepared the way for the immediate cause of death by damage to tissues or impairment of organ function. Underlying cause was defined as the earliest condition that started the sequence between health an death12.
Autopsy procedure and interpretation
External examination, complete autopsy and tissue sampling were performed in 26 patients with COVID-19 and included opening and inspection of all luminal structures and lamellar incisions of all parenchymatous organs. According to recent recommendations for the performance of autopsies in cases of suspected COVID-19, safety precautions including FFP2-masks, protective suits and cut resistant gloves were applied for all autopsies13. For histopathology, representative tissue samples of all organs were fixed in 4% buffered formalin, dehydrated, paraffin embedded and sectioned with a thickness of 4 µm. Paraffin sections were stained with hematoxylin and eosin (HE), periodic acid Schiff’s reaction (PAS), Van Gieson’s elastic stain, Prussian blue stain and Kongo-red stain. At least two pathologists examined all tissue slides by light microscopy.
By autopsy, sepsis or septic organ failure were diagnosed when we observed pathologic–anatomic signs of organ failure, such as severe congestion, necrosis or infarction, together with histologically confirmed signs of infection, i.e. substantial neutrophil rich inflammatory infiltrates or evidence of pathogens. In order to categorize the contribution of identified pathologies to the mechanism of death, we weighed the severity of all findings in each case and determined their causal chains. Findings then were structured as underlying cause, condition leading to cause of death, and immediate cause of death in analogy to WHO guidelines12. We considered COVID-19 as the condition leading to cause of death when it triggered the immediate cause of death sequential to another underlying cause that qualified for initiation of the fatal mechanism. If the pulmonary changes consistent with severe COVID-19 started the sequence of events leading to death this was categorized as the underlying cause. If the pulmonary changes of SARS-CoV-2 infection and COVID-19 were comparably mild or absent, we appreciated this under the category of further relevant conditions.
Statistical analysis
Data collection and statistical analysis were done with IBM SPSS Statistics, Version 23 (IBM, NY, USA). Age at death was presented as median with interquartile range (IQR) to account for deviations from normal distribution. Categorical variables were summarized as counts and percentages. Median time to death was analyzed using the Kaplan–Meier method.
Results
Clinical presentation and causes of death in COVID-19 decedents
We analyzed 26 cases of patients that died after COVID-19 disease and that were autopsied at the Institute of Pathology of the Charité university hospital in Berlin. In all cases, SARS-CoV-2 infection was confirmed by PCR testing. Of the decedents, 17 were male and 9 were female. One of the decedents was of Black ethnicity, while 25 were Caucasians. The median age at death was 70 years (IQR 61.8–78.3, range 30–92 years), and the time from onset of COVID-19 symptoms to death ranged from 5 to 59 days, with a median of 25 days. Additional clinical information on the course of the disease was available in all cases.
Prior to death, all patients had presented with COVID-19 related lung disease. Signs of respiratory failure were most prevalent with 88.5%, while in 57.7% patients had clinical signs of bacterial pneumonia (Table 1). Microbiological records showed bacterial or fungal infection in 15 patients and most patients received treatments with broad spectrum antibiotics (Supplementary Table S1). Furthermore, pulmonary thromboembolism was reported in 23.1% of the cases with clinical evidence of deep venous thrombosis in two patients (7.7%). Due to the severity of lung damage, patient care warranted invasive ventilation in 76.9%, prone positioning in 53.8%, and extracorporeal membrane oxygenation in 30.8% (Table 1). Aside from lung involvement, acute renal failure was the second most prevalent organ failure and hemodialysis was necessary in 69.2% of the patients. Furthermore, half of the patients presented with multi-organ failure, while acute liver failure was reported in 30.8%. These findings indicated severe and complex courses of COVID-19 in these patients. An overview of the clinical characteristics is given in Table 1 and Supplementary Table S1.
To learn about clinical causes of death, we assessed legal death certificates of the 26 decedents. Most frequent immediate causes of death, documented in 19 cases (73.1%), were infection related, and included sepsis, septic shock, or sepsis-related multi-organ failure in 16 cases (61.5%), bacterial infections in two cases (7.7%), and viral pneumonia in one case (3.8%). Second most common were respiration-related causes of death, documented as respiratory insufficiency, hypoxia, or acute respiratory distress syndrome (ARDS) in four cases (15.4%). Further individual immediate causes of death were pulmonary embolism and cardiovascular failure (3.8% each).
In addition, clinical death certificates provided information on conditions leading to immediate causes of death and death-related underlying disease (Table 1). Here, pulmonary disease in 22 decedents (84.6%) was the most frequently documented condition leading to cause of death, which included pneumonia or viral pneumonia in 14 cases (53.8%), and ARDS in eight cases (30.8%). Importantly, when jointly considering conditions leading to cause of death and underlying disease, COVID-19, confirmed or suspected SARS-CoV-2 infection was documented in a total of 23 cases (88.5%), and thus in the vast majority of deceased patients. Other underlying diseases that were deemed clinically relevant for death included cancer in two cases (7.7%), and individual cases of alcohol abuse, renal failure, chronic obstructive pulmonary disease (COPD) or graft-versus-host disease (GvHD). Collectively, these data indicated that, from a clinical perspective, COVID-19 and infection-related disease were major contributors to patients’ death in the majority of cases.
Clinical information on comorbidities
Clinical records also contained information on chronic comorbidities and further relevant health conditions. The median number of chronic comorbidities in these cases was four, and ranged from three to eight (Table 1). Arterial hypertension was the most prevalent chronic condition in the decedents (65.4%), followed by obesity (38.5%), chronic ischemic heart disease (34.6%), atrial fibrillation (26.9%), and chronic obstructive pulmonary disease (23.1%). Vascular conditions were specified as atherosclerosis (7.7%) and cerebrovascular disease (15.4%). Of all patients, 15.4% had diabetes type II, and chronic renal failure was noticed in 11.5% of decedents. Active or non-active nicotine abuse was noted in 5 patients (19.2%) and alcohol abuse in 3 patients (11.5%). Further details and information on related medications are available from Table 1 and Supplementary Table S1, respectively. These data suggested severe chronic comorbidities and health conditions in the majority of patients that had died after COVID-19.
Causes of death determined at autopsy in decedents with COVID-19
In order to investigate causes of death directly, we performed full body autopsies including histopathological workup on all 26 decedents. Based on assessment of pathological disease mechanisms and referring to clinical documentations of death, we defined immediate causes of death, conditions leading to cause of death, and underlying causes (Table 2). As the most common immediate cause of death, we found septic shock and/or multi-organ failure in 8 patients (30.8%), followed by suppurative pulmonary infections in five patients (19.2%), including purulent pneumonia with or without abscess formation, as well as infarct necrosis with signs of superinfection. Right ventricular congestive heart failure or decompensation as immediate cause of death was present in four patients (15.4%). In five patients (19.2%), respiratory failure or diffuse alveolar damage was the immediate cause of death, with severe lung damage implicating highly restricted gas exchange. Four more cases presented with either deadly pulmonary thromboembolism, severe bronchial aspiration, gastrointestinal bleeding, or signs of left ventricular heart failure (3.8% each).
We then determined conditions leading to these immediate causes of death (Table 2). We found that COVID-19 or SARS-CoV-2 infection most prevalently preceded the immediate cause of death in ten cases (38.5%), followed by purulent pneumonia with or without abscess formation in six cases (23.1%), pulmonary bleeding in two cases (7.7%), and arterial thrombosis or thromboembolism also in two cases (7.7%). In addition, we found individual cases with invasive pulmonary mycosis or gastric peptic ulcer as conditions leading to cause of death (3.8% each). Of note, in two cases (7.7%) we did not find pathologies that would qualify for an intermediate between underlying and immediate cause of death.
Next, we identified underlying causes of death, i.e. diseases that initiated the events resulting in death (Table 2). For this, we considered all autopsy findings and the clinical history to determine the underlying disease that would causally explain conditions leading to cause of death and immediate causes of death in all cases. We determined COVID-19 pneumonia as underlying cause of death in the majority of decedents (53.8%). Of note, when considering COVID-19 as underlying cause of death or condition leading to cause of death, this applied to a total of 24 cases (92.3%). Preexisting lung emphysema, pulmonary hypertension, and chronic right ventricular insufficiency were considered as diseases underlying cause of death in 26.9%. In two cases (7.7%), cardiovascular disease, and in two further cases (7.7%), malignant tumors or consequences of tumor therapy were considered as underlying disease. Collectively, our findings demonstrate that septic organ failure, pneumonia, respiratory insufficiency, and right ventricular heart failure due to COVID-19 were the most frequent pathological mechanisms of death in these patients.
Comorbidities found by autopsy in COVID-19 decedents
To learn about other relevant disease conditions in patients that died after SARS-CoV-2 infection, we determined the presence and extent of comorbidities by autopsy (Table 2). Generalized atherosclerosis was present in all but one case (96.2%), and was mild in 9 (34.6%), moderate in 3 (11.5%) and severe in 13 cases (50%). Similarly, coronary artery disease was seen in all but two cases (92.3%), and was mild in 8 (30.8%), moderate in 4 (15.4%) and severe in 11 decedents (42.3%). Furthermore, we noticed preexisting emphysema of the lungs in almost half of the cases (46.2%), and pulmonary artery sclerosis as a sign of pulmonary hypertension in 11 cases (42.3%). Other comorbidities included myocardial hypertrophy (65.4%), hepatosteatosis (11.5%) and liver fibrosis (7.7%). In two cases (7.7%), we defined COVID-19 or SARS-CoV-2 as comorbidity, since we did not observe a direct contribution of this infection to the mechanism of death. These findings demonstrated a high prevalence of cardiovascular and pulmonary comorbidities in patients that had died after COVID-19.
Discussion
Here, we present data on causes of death and comorbidities in patients that had died after a severe course of COVID-19. These patients had reached a median age of 70 years, which in line with previous reports indicates increased risks for fatal COVID-19 outcome with older age14,15. Clinical records showed that in the majority of cases, respiratory insufficiency was a dominating symptom, while the most frequent clinical cause of death was sepsis and thus infection related. Indeed, bacterial or fungal pathogens were found in the majority of cases. In line with these findings, we found by autopsy that sepsis caused by purulent lung infection was the most frequent cause of death, while, in some cases, we observed deadly respiratory insufficiency due to diffuse alveolar damage. These findings suggested that SARS-CoV-2 infection could directly cause lethal lung damage. However, death due to pulmonary bacterial superinfection and sepsis appeared to be a more common causal chain of events that may significantly endanger patients with severe COVID-19-related lung damage. We hypothesize that such causality may be even more prevalent in clinical settings where respiratory insufficiency is manageable by mechanical ventilation or extracorporeal oxygenation. Furthermore, this implies that bacterial infections may contribute to the excessive cytokine release observed in severe COVID-19, which has been termed “cytokine storm”, and may partially explain the similarities of COVID-19 and sepsis16. We therefore suggest that bacterial infections should be kept in mind as a potential confounding variable in studies on inflammatory reactions and cytokine release in COVID-19.
An early autopsy study showed high frequencies of fatal pulmonary thromboembolism in patients that had died of COVID-1910. Deep venous thrombosis was identified as the likely thromboembolic source. In line with these findings, pulmonary thromboembolism was diagnosed in almost every fourth of our patients during the clinical course of the disease. However, we found that pulmonary thromboembolism was an immediate cause of death or a condition leading to cause of death in two cases only, which suggests that in other cases hypercoagulability may have been effectively controlled by anti-coagulant treatment. Nevertheless, hypercoagulability appears to be an important, severe and potentially fatal aspect of COVID-1917,18. Furthermore, peripheral microthrombosis in multiple organ systems has been reported19, which may cause severe organ damage also in patients that survive COVID-19. It therefore remains to be determined by prospective clinical studies, if anti-coagulation reduces the risk of COVID-19 related death, and to what extent this affects the risk of organ damage in COVID-19 survivors.
The majority of deceased patients in our study had diagnosed comorbidities that with arterial hypertension, chronic kidney or heart disease, and chronic pulmonary disease most frequently affected the cardiovascular and respiratory system. By autopsy, we confirmed these clinical diagnoses, since we found their pathological correlates that included general and coronary atherosclerosis, cardiac hypertrophy, and pulmonary emphysema amongst others. In addition, we found a high prevalence of lifestyle risk factors, such as obesity, alcohol consumption, and nicotine abuse. These findings are in agreement with previous studies and imply that patients with preexisting chronic health conditions or lifestyle risk factors are at an increased risk for fatal outcome of COVID-1920,21. However, considering both the high frequency of these comorbidities and the relatively high age of patients that died after SARS-CoV-2 infection, this led to a reasonable debate about the extent to which preexisting health conditions or COVID-19 determined the time of death22, and our data may further inform about this issue. We found that sepsis due to lung infections and respiratory insufficiency were the most frequent immediate causes of death. However, our autopsy series included no single case of immediate deadly ischemic heart disease or stroke, which are the most common causes of death worldwide23, and for which the majority of comorbidities as well as the mentioned life style risk factors that we found were strongly predisposing24. These findings indicate that immediate causes of death were directly linked to lung damage initiated by SARS-CoV-2 infection and not related to preexisting health conditions and comorbidities in most cases.
Conclusion
Our data suggest that in the majority of cases with severe and fatal COVID-19, patients had died of this disease, although in the presence of multiple preexisting health conditions. These findings also support the idea that patients who died of COVID-19 appear to have lost considerable lifetime, independent of their age, as reported by others22. Furthermore, our study highlights the importance of clinical autopsies for a full understanding of novel human disease mechanisms.
A limitation of our study is the relatively small sample size which is insufficient for general associations of clinical management, medications, and patient outcome. Furthermore, patients included in this study had reached a median age of 70 years, which mirrors reported age distributions of inpatient non-survivors in Wuhan14, and data from another autopsy report19, but is lower than suggested by other epidemiologic data from Italy on COVID-19 decedents25. While regional factors may influence age distribution, this discrepancy also suggests a case selection bias, and we speculate this may reflect which patients were hospitalized and therefore received most intense therapeutic measures. The interpretation of autopsy results and conclusions on health impacts of COVID-19 therefore requires careful consideration of the study population.
Data availability
Original data are available upon request.
References
Dong, E., Du, H. & Gardner, L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect. Dis. 20, 533–534. https://doi.org/10.1016/S1473-3099(20)30120-1 (2020).
Organization, W. H. WHO Director-General's remarks at the media briefing on 2019-nCoV on 11 February 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-remarks-at-the-media-briefing-on-2019-ncov-on-11-february-2020 (2020).
Control, E. C. f. D. P. a. COVID-19 situation update for the EU/EEA and the UK, as of 13 June 2020. https://www.ecdc.europa.eu/en/cases-2019-ncov-eueea. (2020).
Wu, Z. & McGoogan, J. M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA. https://doi.org/10.1001/jama.2020.2648 (2020).
Grasselli, G. et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA https://doi.org/10.1001/jama.2020.5394 (2020).
Bartlett, R. H. et al. Initial ELSO guidance document: ECMO for COVID-19 patients with severe cardiopulmonary failure. ASAIO J. 66, 472–474. https://doi.org/10.1097/MAT.0000000000001173 (2020).
Yang, X. et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir. Med. 8, 475–481. https://doi.org/10.1016/S2213-2600(20)30079-5 (2020).
Streeck, H. et al. Infection fatality rate of SARS-CoV2 in a super-spreading event in Germany. Nat. Commun. 11, 5829. https://doi.org/10.1038/s41467-020-19509-y (2020).
Mehra, M. R., Desai, S. S., Kuy, S., Henry, T. D. & Patel, A. N. Cardiovascular disease, drug therapy, and mortality in Covid-19. N. Engl. J. Med. https://doi.org/10.1056/NEJMoa2007621 (2020).
Wichmann, D. et al. Autopsy findings and venous thromboembolism in patients With COVID-19. Ann. Intern. Med. https://doi.org/10.7326/M20-2003 (2020).
Singer, M. et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 315, 801–810. https://doi.org/10.1001/jama.2016.0287 (2016).
Organization, W. H. Medical certification of cause of death: instructions for physicians on use of international form of medical certificate of cause of death. https://apps.who.int/iris/handle/10665/40557. World Health Organization (1979).
Prevention, C. f. D. C. a. Collection and Submission of Postmortem Specimens from Deceased Persons with Known or Suspected COVID-19—Interim Guidance. https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-postmortem-specimens.html.
Zhou, F. et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 395, 1054–1062. https://doi.org/10.1016/S0140-6736(20)30566-3 (2020).
Wu, C. et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern. Med. https://doi.org/10.1001/jamainternmed.2020.0994 (2020).
Zafer, M. M., El-Mahallawy, H. A. & Ashour, H. M. Severe COVID-19 and sepsis: immune pathogenesis and laboratory markers. Microorganisms. https://doi.org/10.3390/microorganisms9010159 (2021).
Klok, F. A. et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb. Res. 191, 145–147. https://doi.org/10.1016/j.thromres.2020.04.013 (2020).
Helms, J. et al. High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study. Intensive Care Med. 46, 1089–1098. https://doi.org/10.1007/s00134-020-06062-x (2020).
Bryce, C., Grimes, Z., Pujadas, E. & Ahuja, S. Pathophysiology of SARS-CoV-2: targeting of endothelial cells renders a complex disease with thrombotic microangiopathy and aberrant immune response. The Mount Sinai COVID-19 autopsy experience. https://doi.org/10.1101/2020.05.18.20099960v1 (2020).
Petrilli, C. M. et al. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. BMJ 369, m1966. https://doi.org/10.1136/bmj.m1966 (2020).
Team, C. C.-R. Preliminary estimates of the prevalence of selected underlying health conditions among patients with coronavirus disease 2019—United States, February 12-March 28, 2020. MMWR Morb. Mortal Wkly. Rep. 69, 382–386. https://doi.org/10.15585/mmwr.mm6913e2 (2020).
Hanlon, P., Chadwick, F., Shah, A. & Wood, R. COVID-19—exploring the implications of long-term condition type and extent of multimorbidity on years of life lost: a modelling study. https://wellcomeopenresearch.org/articles/5-75 (2020).
Organization, W. H. The top 10 causes of death. https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death (2020).
D’Agostino, R. B. Sr. et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation 117, 743–753. https://doi.org/10.1161/CIRCULATIONAHA.107.699579 (2008).
Onder, G., Rezza, G. & Brusaferro, S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA https://doi.org/10.1001/jama.2020.4683 (2020).
Acknowledgements
We are indebted to Anistan Sebastiampillai, Juliane Plaschke and Francisca Egelhofer for excellent technical assistance and helpful advice. There was no external funding for the study.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
S.E., S.G., J.I., E.G.M., P.B., C.A.K., B.V.S., M.G., K.H., B.I.H., F.M., H.H., H.M., H.R., F.L.H. and D.H. performed autopsies, histopathology and clinical workup. V.M.C. made viral RT-qPCR workups. D.H. supervised the study and takes responsibility (acts as the guarantor) for the integrity of the data and the accuracy of the data and analysis. All authors analyzed the data, wrote, revised and approved the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Elezkurtaj, S., Greuel, S., Ihlow, J. et al. Causes of death and comorbidities in hospitalized patients with COVID-19. Sci Rep 11, 4263 (2021). https://doi.org/10.1038/s41598-021-82862-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-82862-5
This article is cited by
-
Sepsis and underlying comorbidities in intensive care unit patients
Medizinische Klinik - Intensivmedizin und Notfallmedizin (2024)
-
Valorization of Salmo salar Skin Waste for the Synthesis of Angiotensin Converting Enzyme-1 (ACE1) Inhibitory Peptides
Waste and Biomass Valorization (2024)
-
Clinical features and 28-day mortality predictors of vaccinated patients admitted to a COVID-19 ICU hub in Italy
Journal of Anesthesia, Analgesia and Critical Care (2023)
-
Associated organs and system with COVID-19 death with information of organ support: a multicenter observational study
BMC Infectious Diseases (2023)
-
A prospective study of extraesophageal reflux and potential microaspiration in patients hospitalized with COVID-19 in Jordan
BMC Pulmonary Medicine (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.