Abstract
This consensus statement established under the auspices of the German working group on BM and blood stem cell transplantation (DAG-KBT), the German Society of Hematology and Oncology (DGHO), the Austrian Stem Cell Transplant Working Group, the Swiss Blood Stem Cell Transplantation Group (SBST) and the German-Austrian Pediatric Working Group on SCT (Päd-Ag-KBT) summarizes current evidence for diagnosis, immunosuppressive and supportive therapy to provide practical guidelines for the care and treatment of patients with pulmonary manifestations of chronic GVHD (cGVHD). Pulmonary cGVHD can present with obstructive and/or restrictive changes. Disease severity ranges from subclinical pulmonary function test (PFT) impairment to respiratory insufficiency with bronchiolitis obliterans being the only pulmonary complication currently considered diagnostic of cGVHD. Early diagnosis may improve clinical outcome, and regular post-transplant follow-up PFTs are recommended. Diagnostic work-up includes high-resolution computed tomography, bronchoalveolar lavage and histology. Topical treatment is based on inhalative steroids plus beta-agonists. Early addition of azithromycin is suggested. Systemic first-line treatment consists of corticosteroids plus, if any, continuation of other immunosuppressive therapy. Second-line therapy and beyond includes extracorporeal photopheresis, mammalian target of rapamycin inhibitors, mycophenolate, etanercept, imatinib and TLI, but efficacy is limited. Clinical trials are urgently needed to improve understanding and treatment of this deleterious complication.
Similar content being viewed by others
Introduction
Chronic GVHD (cGVHD) is still a major complication of long-term survivors after allo-HSCT, with a 6-year probability up to 61% in patients receiving PBSC.1, 2, 3 Owing to the increasing number of allo-HSCTs using PBSCs, mismatched and unrelated donors, the clinical application of donor lymphocyte infusions or allo-HSCT in elderly or very young patients, cGVHD will become an even more common and serious challenge in the clinical follow-up after transplantation. In addition to its related mortality, several surveys show that active cGVHD markedly reduces the quality of life in patients suffering from the moderate or severe form.4, 5, 6
Pulmonary complications significantly contribute to late mortality after allo-HSCT. In patients surviving longer than 2 years, Bathia et al.2 found a 15.1-fold increased risk of late mortality because of pulmonary dysfunction compared with the general population. Furthermore, late-onset non-infectious pulmonary complications can present with restrictive lung function impairment (restrictive pulmonary function test (PFT) pattern, late interstitial pneumonitis (IP), cryptogenic organizing pneumonia (COP) also called bronchiolitis obliterans organizing pneumonia (BOOP)), or airway obstruction (obstructive PFT pattern, bronchiolitis obliteratans (BO) or BO syndrome (BOS)) or a combination of both.7, 8, 9 Late-onset non-infectious pulmonary complication forms are strongly associated with cGVHD and not pathophysiologically fully understood.7, 8, 9, 10, 11, 12, 13, 14, 15 However, BO/BOS is the only pulmonary complication, which is currently considered diagnostic of cGVHD,16 whereas BOOP can also be detected in acute GVHD and, therefore, is regarded as a ‘common’ symptom of GVHD. Late IP as well as COP may occur in association with cGVHD and are regarded as ‘associated’ or ‘other’ symptom of cGVHD. BO/BOS is the most detrimental post-transplant late pulmonary complication, as it is characterized by its frequent non-responsiveness to treatment and irreversibility, leading to high morbidity and mortality. A comprehensive review on this entity has been recently published by Williams et al.17
The Consensus Conference on Clinical Practice in Chronic GVHD was held in Regensburg, Germany on 6th and 7th November 2009 (http://www.gvhd.eu). It aimed to summarize the currently available evidence for diagnosis, immunosuppressive and supportive treatment of pulmonary manifestations and to provide practical guidelines for the use of treatment modalities. The Consensus Conference was organized under the auspices of the German working group on BM and blood stem cell transplantation (DAG-KBT) and the German Society of Hematology and Oncology (DGHO), the Austrian Stem Cell Transplant Working Group of the Austrian Society of Hematology and Oncology, the Swiss Blood Stem Cell Transplantation Group (SBST) and the German-Austrian Pediatric Working Group on SCT (Päd-Ag-KBT). It was based on a review of published evidence and two surveys on the current clinical practice in diagnosis and treatment of cGVHD including BO. In total, 31 transplant centers from Germany, Austria and Switzerland participated in the surveys. Moreover, the consensus was circulated among all transplant centers performing allo-HSCT in Germany, Austria and Switzerland, and was discussed during the Consensus Conference meetings.
The literature search was performed by the working group on first-line treatment within the Consensus conference using the PubMed database. Only English literature was considered. Abstracts from the Bone Marrow Transplantation Tandem meetings, the European Bone Marrow Transplantation meetings and the American Society of Hematology meetings were cited but were not included in the evidence rating. The evaluation of evidence and the subsequent recommendation was graded according to the system used in grading of supportive care published by Couriel et al.18 As the evidence of the majority of treatment options in cGVHD is sparse and therefore the strength of recommendation falls into category C for most of the therapeutic options; the category C and evidence III level were further specified as shown in Tables 1 and 2. All strength of recommendation and evidence levels were first rated by an expert panel and subsequently rated by all the participants of the consensus process. Only evidence from the use in cGVHD was included in the evaluation.
Following this, we discuss the diagnostic criteria, screening methods, systemic and topical immunosuppressive treatment options for pulmonary manifestations of cGVHD. We mainly focus on reported clinical trials and retrospective analyses. The presented overview on current evidence and the herein deduced recommendations by the Consensus Conference participants are intended to provide a platform for collaborative efforts in order to plan and pursue clinical trials directed to disease pathophysiology, treatment and outcome.
Diagnosis
I. Symptoms of pulmonary cGVHD
In the early stage, patients with pulmonary cGVHD are either asymptomatic or often present with nonspecific and non-diagnostic symptoms such as mild dyspnea on exertion or dry and non-productive cough. Owing to the initial lack of the patient's perception of disease, the detection of disease is usually delayed until airflow patterns and lung structure have significantly changed, and patients suffer from significant dyspnea from exertion, decreased exercise tolerance and exhibit a more eminent persistent non-productive cough. Fever (indicating associated infection), dyspnea and productive vs non-productive cough can be found in any combination or not at all.14, 19, 20, 21, 22, 23, 24, 25, 26 If pulmonary disease progresses, eventually oxygen dependency, immobility and death will occur mainly in association with pulmonary infectious complications.
II. Medical history and physical examination
On the basis of the patient's delayed perception and the nonspecificity of clinical symptoms and findings on physical examination, a standardized approach is necessary to detect pulmonary cGVHD early and—if possible—before irreversible structural changes have occurred. In addition, infectious causes need to be ruled out to the best extent. Proof of underlying viral, bacterial and fungal disease requires targeted antimicrobial and antiviral treatment, whereas in pulmonary cGVHD, starting or intensifying immunosuppression is the mainstay of therapy, which is often contraindicated in the presence of infection.
Therefore, the following medical history and laboratory work-up is suggested: donor type (unrelated vs sibling), HLA match/mismatch, use of TBI or BU, history of donor lymphocyte infusion, donor and patient gender (female donor—male recipient), patient age, CMV seropositivity of donor and recipient, history of smoking, allergies, chronic infectious complications, lung disease or thoracic irradiation pre-HSCT, history of acute lung injury following allo-HSCT, history of cGVHD at any other site, complete WBC count including differential for eosinophilia and serum Ig levels (IgG and IgA).10, 11, 19, 27, 28, 29, 30, 31 A thorough physical examination including heart and lung has to be performed on each patient visit including the evaluation for any signs or symptoms of cGVHD at other sites. An additional echocardiography to address pulmonary artery pressure and a standardized oxygenation assessment as suggested by the current guidelines of the American Thoracic Society, for example, 6-min-walk test, are further recommended.17, 32
III. Pulmonary function testing
PFTs by spirometry, whole-body plethysmography and the single-breath CO method are a non-invasive, easy-to-do approach to assess pulmonary function following allo-HSCT in adults.33 In early childhood, cooperation is often limited and reliable PFT results can only be achieved from the age of 5 years. Baby plethysmography in sedation is a rarely necessary option for testing pulmonary function in infants. Despite no apparent respiratory symptoms, many patients develop normal-to-mild restriction (normal or reduced forced expiratory vital capacity (FVC) or total lung capacity (TLC) in combination with increased residual volume (RV)/TLC ratios and normal to mildly reduced flow rates, suggesting that functional and structural changes occur before clinical symptoms and physical impairment become manifest.34 Further, impaired pulmonary function reflected by either decreased TLC, FVC, diffusion capacity of the lung for carbon monoxide or forced expiratory volume at 1 s (FEV1) or an increase of the calculated lung function score (LFS) at day 80 post SCT has been associated with higher mortality and decreased survival.35 Specifically for BO/BOS, the National Institutes of Health consensus defined mild BO/BOS, which is often asymptomatic, as a manifestation of cGVHD, which already requires systemic treatment,18 and moderate BO/BOS—like other moderate-to-severe organ manifestations of cGvHD—relates to impaired physical functioning and decreased quality of life.36 BO/BOS can occur at any time (mostly during the first 2 years following allo-SCT). In order to identify patients at risk for pulmonary cGVHD or to detect manifest subclinical disease early, screening seems justified and has been made a consensus recommendation of this group as it has also been recommended by the National Institutes of Health Ancillary Therapy and Supportive Care Working Group.18 Successful screening may be most easily warranted by using a standardized lung function analysis approach, and the following approach may be considered: Baseline PFT within the last 2 weeks before starting conditioning therapy, and as follow-up every 3 months for the first 2 years after transplantation and every 6 months thereafter.37 Additional PFTs are needed when patients present with respiratory symptoms in the absence of acute pulmonary infection or 2–4 weeks after initiation of treatment following pathological PFTs.
Indicators of a restrictive spirometric pattern are VC or TLC <80% or FVC <80% of predicted value in combination with forced expiratory volume in the first second of expiration (FEV1)/FVC ⩾0.7.10, 23 Although restrictive lung function changes can be easily quantified by PFT in patients after allo-HSCT, a correct assessment of true airflow obstruction and its most deleterious form, BO, is more difficult. According to the current guidelines of the ATS/ERS taskforce, FEV1 can be used to measure the severity of obstructive as well as restrictive changes in pulmonary function, as each concurs with a decrease in FEV1.38 Further, in patients following allo-HSCT, multiple factors such as conditioning regimen toxicity, scleroderma-like cGVHD or steroid treatment-related myopathy can lead to intrinsic or extrinsic pulmonary restriction. When applying the FEV1/FVC ratio as parameter for obstructive airway disease, values appear falsely normal despite manifest pulmonary obstruction in the presence of significant restriction.39, 40 A decline of FEV1 higher than 5% per year in combination with a FEV1/FVC <0.8 has been demonstrated indicative of airflow obstruction following allo-HSCT.25 Therefore, it is suggested, that FEV1 values will be compared over time in order to detect obliterative airway disease early at a time point, when pulmonary damage may still be reversible. In these patients, reversibility of obstructive changes can be addressed by the effects of bronchodilator administration (significant bronchodilator responses (FEV1 or FVC increase ⩾12% or 0.2 L from pre-bronchodilator)).41, 42 In addition, the combination of FEV1 <75% of predicted normal in combination with a FEV1/FVC <0.7 may be of higher validity as a PFT indicator for BO than each parameter alone.16 In children, the measured effective resistance (Reff) can be additionally used as indicator of mild (30–60% of predicted normal), intermediate (60–100%) or severe (>100%) restrictive ventilatory disorder.
The transfer factor of the lungs for carbon monoxide (TLCO) or diffusion capacity measures the ability to exchange gases at the alveolar capillary interface and reflects alveolar membrane thickness. However, it may be affected by Hb levels as well as by cardiac output, and shows the highest variability between laboratories. In pediatric populations, correction for Hb levels is not generally recommended. Furthermore, reproducible TLCO measurement is only feasible from the age of 10 years, because an expiration time of 10 sec is needed for this test, requiring optimal cooperation. The relevance of TLCO decreases after allo-HSCT is unclear, as a decline in TLCO is apparent in up to 80% of all HSCT survivors, may reflect alveolar–endothelial damage or subclinical fibrosis and has been associated with improved or decreased survival, as no association at all has been reported as well.23, 30, 43, 44, 45, 46
The lung function score (LFS) combines FEV1 and the TLCO in an equally distributed manner (FEV1: >80%=1, 70–79%=2, 60–69%=3, 50–59%=4, 40–49%=5, <40%=6; TLCO (corrected for Hb levels): >80%=1, 70–79%=2, 60–69%=3, 50–59%=4, 40–49%=5, <40%=6; summary score (FEV1+TLCO): ⩽2=LFS I, 3–5=LFS II, 6–9=LFS III, 10–12=LFS IV).47 The LFS was first proposed by Parimon et al.48 as a potentially better approach to correlate PFT before allo-HSCT with clinical outcome. It was then revisited and modified into more precisely subdividing subcategories by the National Institutes of Health consensus development project on criteria for clinical trials in cGVHD and suggested as a score to quantify pulmonary cGVHD and to evaluate the effect of cGVHD treatment in adults.47 No validated LFS exists for children so far, hence LFS is not a recommended tool for the evaluation of pulmonary cGVHD in childhood. Further, at this time the LFS has not been validated yet in its proposed form, but we suggest its inclusion in the follow-up of every adult patient in this setting for further evaluation.
A further diagnostic option seems to be measurement of the fraction of exhaled nitric oxide, which has been shown to have a potential predictive value for BO in adults.49 However, different age-dependent norm values have to be considered in adults (normal 5–25 p.p.b., intermediate 25–50 p.p.b., high >50 p.p.b.) and children (normal 5–20 p.p.b., intermediate 20–35 p.p.b, high >35 ppb or a rise of >60% since previous measurement). Fraction of exhaled nitric oxide measurements can usually be performed from the age of 4 years with a portable device.
In the performed survey on diagnosis of cGVHD, only half of the participating centers stated performing lung function screening of asymptomatic patients. As a result of the consensus conference, all centers agreed to establish routine pulmonary function testing at certain time points because of the fact that symptomatic BO already significantly interferes with quality of life and physical functioning and therefore screening of asymptomatic patients is required.
IV. Imaging studies
Conventional chest X-ray presents a fast and easy method to determine the likelihood of an infectious vs non-infectious etiology, when classical radiographical signs of lobar or bronchial bacterial pneumonia are present and match clinical findings. However, its sensitivity and specificity are limited when compared with chest CT, and the latter should be alternatively considered according to the clinical setting and institutional policies. If non-infectious lung injury is suspected and differentiation from viral or fungal pneumonia is necessary, high-resolution chest computed tomography (HRCT) is recommended as the standard imaging technique for addressing lung injury in adult SCT recipients. In young children up to the age of about 10 years, sedation can be necessary for the performance of a chest CT, making the evaluation of inspiration and expiration difficult. Therefore, early multislice CT scan (if possible with expiration) may be considered in children as long as lung injury has not progressed, which may increase the risk of sedation. In most cases with COP or BOOP, patchy consolidation and ground-glass attenuation are seen as characteristic findings.50 In- and expiratory HRCT studies in cooperative patients are very helpful in the assessment of obstructive lung injury, which presents with bronchial dilatation, mosaic pattern of attenuation and air trapping, and correlates with PFT parameters, including FEV1, FEV1/FVC, RV and TLCO, but not with TLC or with FVC.50, 51 Furthermore, HRCT provides information regarding potential infectious etiology of lung injury, demonstrating a higher specificity for fungal vs viral or bacterial infections.52, 53
In patients with clinical symptoms of sinus infection and suspected sinobronchial syndrome, a CT of the sinuses is suggested to explore potential foci, driving pulmonary infections, and may be also strongly considered even in younger children. In the survey on diagnosis of cGVHD all but one of the participating centers stated performing routine HRCT scans in patients with a drop of the FEV1 and suspicion of pulmonary cGVHD.
V. Bronchoalveolar lavage
Respiratory symptoms and pathological findings by HRCT require further work-up by bronchoalveolar lavage (BAL) to define or exclude causative infectious agents. BAL is recommended early and in all patients for various reasons: (1) proof or exclusion of infection significantly effects subsequent therapy, (2) pulmonary function may rapidly decline and invasive ventilator support may become necessary.
We suggest, that BAL cytology analysis incorporates absolute cellularity as well as leukocyte sub-populations, CD4:CD8 ratio and atypical epithelial cells by morphology and FACS.54 Screening for infection commonly involves stains, cultures and/or PCR for bacteria, viruses and fungi. Specific pathogens of interest include pneumococci, Haemophilus influenzae B, Chlamydia pneumoniae, Mycoplasma pneumoniae, Toxoplasma gondii, Bordetella pertussis, Mycobaterium tuberculosis and mycobacteria other than tuberculosis, Pneumocystis jirovecii, adenovirus, CMV, HHV6, HSV1/2, human metapneumovirus, influenza A/B, parainfluenza 1–3, coronavirus, rhinovirus, respiratory syncytial virus and Aspergillus species. In individual cases, pan-bacterial or pan-fungal PCR screening may be indicated.
No controlled study on the benefits, risks and value of BAL in patients with pulmonary cGVHD has been reported yet. However, as BAL has been shown to be a well tolerated and safe procedure even in pediatric populations, with a high informative value in patients with acute pulmonary dysfunction following allo-HSCT,55 it seems also safely applicable to patients at later time points. In the survey on diagnosis of cGVHD only one-third of the participating centers stated performing BAL in patients with a drop of FEV1. If radiological signs of pulmonary cGVHD are present, the majority of centers stated performing BAL as a diagnostic procedure.
VI. Transbronchial biopsy and open lung biopsy
Definitive diagnosis of different forms of pulmonary cGVHD needs histopathological confirmation. Transbronchial biopsy may be helpful in diffuse lung pathology with typical HRCT findings such as ground-glass appearance or fibrosis or when lesions larger than 1 cm are located in very close proximity to major bronchi, whereas open lung biopsy may be considered in patients with small focal processes located in the peripheral lung parenchyma. Although transbronchial biopsy is associated with low sensitivity and with a relatively poor predictive value for BO,56 its value is higher in patients with late IP. In contrast, open lung biopsy remains the gold standard for the diagnosis of BO or COP/BOOP, but at the same time it is associated with an overall morbidity of 43% by day +30 after the procedure, and can result in severe and life-threatening complications in every seventh patient.57, 58 Therefore, the decision, whether a transbronchial or an open lung biopsy may be performed, has to be made carefully on a case by case base in the context of radiographical findings, the risk of potential complications and the expected clinical consequences to be made depending upon biopsy results, but still be pursued consequently. In the survey on diagnosis of cGVHD only half of the participating centers stated performing transbronchial lung biopsies during diagnostic work-up for cGVHD. In this connection, the need for experienced second-opinion pathologists was stated to improve the quality of histological diagnosis of pulmonary cGVHD.
Establishing the diagnosis of BO/BOS
In 2005, the consensus project on cGVHD of the National Institute of Health, USA, has provided a definition for BO/BOS, which is primarily based on PFT and HRCT, and requires the following criteria16 in order to characterize BO/BOS as a manifestation of cGVHD:
-
1)
FEV1 <75% of predicted normal and FEV1/FVC <0.7.
-
2)
Either signs of air trapping by PFT (RV >120% of predicted normal) or signs of air trapping, small airway thickening or bronchiectasis by in- and expiratory HRCT or pathological confirmation of constrictive bronchiolitis.
-
3)
Absence of active respiratory tract infection.
-
4)
In case of lacking histological proof of BO, at least one other distinctive manifestation of cGVHD in an additional organ system is required.
The International Consensus Conference on diagnosis and treatment of cGVHD of the German, Austrian and Swiss transplantation groups agreed to apply this definition in clinical routine and clinical trials. For pediatric patients, however, the requirement of cGVHD involvement of other organs besides lung in the absence of histological proof of BO may not be seen as stringent, as performing biopsies in these patients is often clinically impossible, and isolated BOS can be observed frequently without other organ cGVHD.59 A less stringent modification of these criteria has been recently proposed to potentially broaden the inclusion of patients into clinical trials.60
Treatment of pulmonary cGVHD
In early BO, bronchiolar inflammation has been shown to be present,39, 61 and therefore, early treatment may prove more promising than initiation of therapy once structural, fibrotic changes have occurred. When FEV1 drops more than 5% within the last year in combination with a FEV1/FVC <0.8,25 or when FEV1 <80% (GOLD I) with FEV1/FVC >0.7, and no air trapping by PFT or HRCT can be found by PFT or HRCT, or when patients have a LFS of ⩽II and present with no or mild clinical symptoms, the indication for topical treatment (Table 3) is given.
Bergeron et al.62 retrospectively analyzed the role for topical treatment early in the course of progressive airflow obstruction using a combination of budenoside as an inhalative steroid and formoterol as a long-acting bronchodilator. A total of 13 patients with mild-to-moderate BO were treated with this regimen and showed a durable improvement both clinically and in PFTs over the follow-up of 12.8 months (5–29 months). This combined regimen may be a promising approach (B III-2). Currently a prospective trial evaluating the efficacy of budesonide and formoterol in treatment of BO after allo-HSCT is ongoing.63 In contrast to the results in BO after lung transplantation, a recently published retrospective analysis on inhaled high-dose fluticasone in treatment of BO after allo-HSCT showed some efficacy in a group of 17 patients.64 However, when inhaled corticosteroids (ICS) are used as topical antiinflammatory treatment as recommended for children, fluticasone or ciclesonide may be considered in combination with short-acting beta-agonists as salbutamol rather than with long-acting beta-agonists, as the latter are not recommended in infants or toddlers.
In the survey, 27 of 31 centers stated using the combination of inhalative and systemic steroids, whereas six centers applied systemic steroids only. Two centers used both options. With regard to the use of inhalative bronchodilators, seven centers stated using short-acting sympathomimetic inhalative agents. In total, 24 centers use long-acting sympathomimetic agents and eight centers apply parasympatholytic agents. Four centers did not use one of both options.
In pediatric and adult patients, the use of dornase alpha inhalations65 may be considered, if a sinobrochial syndrome or chronic mucus plugging with suspected mucociliary dysfunction is present, leading to further infections and bronchiectasis. In case of chronic bacterial colonization of the airways, inhalation with tobramycin can be considered.
Pulmonary hypertension may develop if chronic restrictive airway disease is persisting. In these patients, inhalative iloprost may be a therapeutic option.66, 67
Following 2- to 4-weeks of treatment, the patient needs to be re-evaluated. If no improvement or even progressive disease is observed, initiation of systemic immunosuppression (Table 3) is suggested. We recommend, that systemic immunosuppressive therapy may also be started up-front in those patients initially presenting with moderate-to-severe clinical symptoms, a LFS >II, a FEV1 <75% in combination with a FEV1/FVC <0.7 or when air-trapping is present by PFT or HRCT.
First-line treatment usually involves corticosteroids, for example, prednisolone 1 mg/kg body weight (A II) (maximum 100 mg prednisolone/day) plus, if any, continuation of other immunosuppressive therapy, for example, calcineurin inhibitors, and clinical responses can be observed in about one-fifth of patients.13, 25, 68, 69 Alternatively, steroid pulse treatment with prednisolone at a dose of 10 mg/kg body weight/day for 3 days can be applied (C-2 III-2).70 In this study, a median number of four cycles was given with a 4-week interval between cycles. FEV1 improved after 2 months of treatment and disease progression was halted in 5/9 patients over a mean follow-up for 4219, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67 months.70 Steroids also present standard first-line treatment for restrictive late-onset non-infectious pulmonary complications, including COP/BOOP and late IP, and are given at a dose of at least prednisolone 1 mg/kg body weight (A II).14 As in most cases, this leads to improvement or stabilization of disease,14 and tapering steroids can be usually initiated after 2 weeks of treatment.
However, treatment success specifically for BO often does not persist, and other immunosuppressive drugs or immunomodulatory approaches become necessary. Extracorporeal photopheresis has been reported with some success in the treatment of cGVHD including BO in several studies (C-1 III-1) and also in the treatment of COP.71, 72, 73, 74, 75 Response rates up to 40 and 67% for restrictive and obstructive lung involvement, respectively, have been reported.76, 77, 78 Interestingly, a recent study demonstrated a response in about two-thirds of patients, who suffered from refractory BO, despite a median number of five treatment approaches.78 However, criteria for pulmonary cGVHD so far have not been uniformly defined and patient numbers in general are low, and larger prospective studies are needed to better determine the role of extracorporeal photopheresis in the treatment of cGVHD-related lung disease.
Although efficacy for calcineurin inhibitors, such as CyA or tacrolimus, mammalian target of rapamycin inhibitors, such as sirolimus and everolimus, or mycophenolate mofetil has been shown in patients with BO following lung transplant,79, 80, 81, 82, 83 and these substances are frequently used in treatment of cGVHD,84, 85 usage of these drugs in patients with BO after allo-HSCT remains empirical, as no clinical trials exist. Replacement strategies, for example, changing from CyA to tacrolimus82 or combinative approaches such as CyA plus mycophenolate mofetil83 or sirolimus plus mycophenolate mofetil,79 may prove beneficial in HSCT recipients and warrants further investigation. However, in light of their common clinical use outside of trials for patients with BO after allo-HSCT and the mainly unchanged clinical outcome, the ability and efficacy of these drugs to significantly alter the progressive course of disease has to be seen critically, even more as additional immunosuppressive measures need to be balanced against an increased risk of opportunistic infections.
In small case series, azithromycin, a macrolide antibiotic, showed potency with high efficacy and low toxicity in the treatment of BO following lung transplantation.86, 87, 88 However, there has been only one report published on azithromycin and BO following HSCT.89 In this study, 8/153 patients had developed BO after HSCT (seven allo, one auto) and were treated with azithromycin 500 mg q.d. for 3 days, followed by 250 mg 3 × /week for 12 weeks. Clinically significant improvement was achieved in both FEV1 and FVC in seven out of eight patients. Therefore, azithromycin provides a well-tolerated therapeutic approach and we recommend its routine use in patients with mild airflow obstruction in addition to topical therapy (C-1 III-2). Further, it is recommended to continuously add azithromycin to other immunosuppressants such as CyA or steroids in patients with moderate and severe obstructive lung disease. Although the mechanism of action for azithromycin is not fully understood, it seems that it not only leads to a reduction of neutrophilc inflammation88, 90 but also functions through its prokinetic properties on the upper gastrointestinal tract, thereby reducing gastroesophageal reflux, a recently established risk factor for BO.91, 92
Interestingly, two different forms of BO have been described, that can be discriminated by their response to azithromycin: a responsive neutrophilic partially reversible and a non-responsive fibroproliferative form,88, 93 and further research may aid in understanding, whether these confer to the neutrophilic vs lymphocytic form of BO, described two decades ago,94 or present different stages of disease.
TNF is a critical factor in the development of acute lung injury following allo-HSCT, and neutralization significantly improves clinical outcome in those patients.95 However, the role of TNF in the development of pulmonary cGVHD has not been established, and anti-TNF treatment is still fully investigational. So far, the successful use of TNF blockade has been reported only in case reports both for infliximab (C-4 III-3) in BO96 and for etanercept (C-4 III-3) in late IP,97 and its use remains experimental and we recommend its restriction to special circumstances because of the associated infectious risk.
Profibrotic cytokines and receptors are significantly involved in the pathophysiology of BO, BOOP and other fibrotic manifestations of cGVHD.98, 99, 100, 101 Therefore, targeting fibrosis presents a promising therapeutic approach and has led to the use of the tyrosine kinase inhibitor imatinib in patients with pulmonary cGVHD based on its antifibrotic properties.102, 103, 104, 105, 106 Majhail et al.102 reported one patient with BO, who demonstrated a significant and durable response to imatinib at a dose up to 400 mg daily for more than 5 years. In patients with combined obstructive–restrictive chronic lung injury, imatinib (100–400 mg daily) led to a significant improvement in lung function following a treatment period of 6 months in 6 out of 11 cases.103 Imatinib was combined with concurrent immunosuppression in both studies, and in future may prove an efficient additive arm of treatment in patients with pulmonary cGVHD. Currently, imatinib may be considered as additive agent in second-line treatment of BO (C-2 III-1).
Both restrictive and obstructive forms of lung injury following allo-HSCT are the result of persistent and dysregulated inflammation. Leukotrienes are eicosanoid lipid mediators, that contribute to the inflammatory processes involved in the development of asthma, alveolitis, pulmonary fibrosis and BO following lung transplantation, and promote bronchoconstriction as well as eosinophil and neutrophil recruitment.107, 108, 109, 110, 111 Preliminary clinical observations demonstrated potential therapeutic efficacy for montelukast, a leukotriene receptor antagonist in patients with BO following allo-HSCT,112 and is currently tested by an ongoing National Institutes of Health phase 2 trial. In addition, combined treatment with fluticasone, azithromycin and montelukast demonstrated comparable efficacy as prednisone in stabilizing FEV1 in patients with BO, but allowed a significant reduction in total dose prednisone exposure, thereby may proof as an steroid sparing treatment alternative in this disease.113 Currently, montelukast may be considered as additive agent in treatment of BO (C-2 III-1).
TLI and inhalative CyA present treatment options, which have been successfully used in small numbers of patients with BO after lung transplantation, but their use has not yet been reported for patients with BO after allo-HSCT.114, 115, 116, 117, 118, 119, 120 Therefore, the use of these treatment modalities may be considered experimental and used in clinical trials or in individual cases only (C-4).
When medical treatment fails to prevent the progression of pulmonary disease, eventually lung transplantation as the therapeutic ultima ratio may be indicated. Several reports have demonstrated the clinical efficacy and value of this procedure in adult HSCT recipients.121, 122, 123, 124, 125, 126 The indication for lung transplantation, including progressive deterioration despite immunosuppression for more than 3–6 months, acute respiratory distress, total dependence on oxygen support, severe limitation in exercise and life quality because of lack of oxygen or severe pulmonary hypertension, has to be counterbalanced with the general state of health and age of the patients and with transplantation-associated limitations, such as risk of relapse, infections or secondary neoplasia because of prolonged immunosuppression following lung transplantation.
In the survey on treatment of cGVHD, all centers agreed on the central role of systemic steroids in treatment of pulmonary GVHD. Moreover, 16 of 31 centers apply a pulse of steroids during the course of BO with six centers applying at time of diagnosis of pulmonary cGVHD and four centers using it second line. Calcineurin inhibitors are applied by 24 centers with 24 centers using CyA and 13 centers using also tacrolimus. The majority of centers regard calcineurin inhibitors as second- and third-line treatment option. Mycophenolate mofetil is used by 21 centers in treatment of BO with the majority applying it as second- and third-line therapies. Extracorporeal photopheresis is applied by 15 of 31 centers in the treatment of BO>w> mainly as third- and fourth-line treatment options. The mammalian target of rapamycin inhibitors sirolimus (10 centers) and everolimus (11 centers) are applied mainly after failure of first-line treatment and were regarded as treatment of first choice by two centers.
Imatinib is currently applied by four centers only in more advanced treatment lines. Etanercept is considered by six centers mainly as third- and fourth-line treatment. Azathioprine, pentostatin, infliximab and basiliximab are applied by 2 of 31 centers only.
Summary
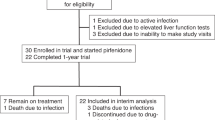
The diagnostic complexity and the vast variety in the choice and algorithm of treatment approaches between centers reflects the current dilemma of pulmonary cGVHD: until today, criteria and definitions of cGVHD of the lung have not been uniformly applied; the clinical spectrum reaches from subclinial PFT changes to severe, life-threatening pulmonary impairment; the knowledge of when and how to treat has rather been based on anecdotal experiences or small numbered case series from single centers than on data derived from clinical multicenter trials and treatment may often be started too late at a time point when irreversible structural remodeling of the pulmonary parenchyma has occurred. Translating the conclusions and recommendations of this Consensus Statement into routine diagnostics, clinical care and follow-up of patients after allo-HSCT (Figures 1 and 2) may help to achieve a more uniform treatment of disease at different HSCT centers, therefore allowing a better assessment of response data and comparability of experiences, as well as an optimization of patient care. Better experimental models may help improving the understanding of pulmonary cGVHD pathophysiology127 and future clinical multicenter trials addressing risk factors, patient management and follow-up, as well as evaluating specific therapeutic options (e.g., in order to better define the role of extracorporeal photopheresis vs azithromycin as added treatment option to first-line steroids) are eagerly needed.
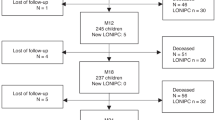
Diagnostic and clinical care work-up algorithm for lung injury following allo-SCT. (1) Routine PFT screening is recommended 3, 6, 9, 12, 18 and 24 months after allo-SCT and then once per year. (2)Impaired PFT should be at least a drop in FEV1 >5% over the last 12 months or a LFS ⩾2 or a FEV1 <80% (GOLD I) with FEV1/FVC >0.7. (3) The decision, whether a transbronchial or an open lung biopsy may be performed, has to be made carefully on a case by case basis in the context of radiographical findings, the risk of potential complications and the expected clinical consequences to be made depending upon biopsy results.
References
Abou-Mourad YR, Lau BC, Barnett MJ, Forrest DL, Hogge DE, Nantel SH et al. Long-term outcome after allo-SCT: close follow-up on a large cohort treated with myeloablative regimens. Bone Marrow Transplant 2010; 45: 295–302.
Bhatia S, Francisco L, Carter A, Sun CL, Baker KS, Gurney JG et al. Late mortality after allogeneic hematopoietic cell transplantation and functional status of long-term survivors: report from the Bone Marrow Transplant Survivor Study. Blood 2007; 110: 3784–3792.
Schmitz N, Eapen M, Horowitz MM, Zhang MJ, Klein JP, Rizzo JD et al. Long-term outcome of patients given transplants of mobilized blood or bone marrow: a report from the international bone marrow transplant registry and the European group for blood and marrow transplantation. Blood 2006; 108: 4288–4290.
Chiodi S, Spinelli S, Ravera G, Petti AR, Van Lint MT, Lamparelli T et al. Quality of life in 244 recipients of allogeneic bone marrow transplantation. Br J Haematol 2000; 110: 614–619.
Fraser CJ, Bhatia S, Ness K, Carter A, Francisco L, Arora M et al. Impact of chronic graft-versus-host disease on the health status of hematopoietic cell transplantation survivors: a report from the Bone Marrow Transplant Survivor Study. Blood 2006; 108: 2867–2873.
Kiss TL, Abdolell M, Jamal N, Minden MD, Lipton JH, Messner HA . Long-term medical outcomes and quality-of-life assessment of patients with chronic myeloid leukemia followed at least 10 years after allogeneic bone marrow transplantation. J Clin Oncol 2002; 20: 2334–2343.
Cooke KR, Hildebrandt GC . Pulmonary toxicity following hematopoietic cell transplantation: is the lung a target organ of graft-versus-host disease? Curr Opin Organ Transplant 2006; 11: 69–77.
Tichelli A, Rovo A, Gratwohl A . Late pulmonary, cardiovascular, and renal complications after hematopoietic stem cell transplantation and recommended screening practices. Hematology Am Soc Hematol Educ Program 2008, 125–133.
Bolanos-Meade J, Chien J . Chronic graft versus host disease and the lung. In: Vogelsang, GB and Pavletic, SZ (eds). Chronic Graft Versus Host Disease: Interdisciplinery Management, Vol. 229. Cambridge University Press: Cambridge, UK, 2009, p 37.
Patriarca F, Skert C, Sperotto A, Damiani D, Cerno M, Geromin A et al. Incidence, outcome, and risk factors of late-onset noninfectious pulmonary complications after unrelated donor stem cell transplantation. Bone Marrow Transplant 2004; 33: 751–758.
Sakaida E, Nakaseko C, Harima A, Yokota A, Cho R, Saito Y et al. Late-onset noninfectious pulmonary complications after allogeneic stem cell transplantation are significantly associated with chronic graft-versus-host disease and with the graft-versus-leukemia effect. Blood 2003; 102: 4236–4242.
Savani BN, Montero A, Srinivasan R, Singh A, Shenoy A, Mielke S et al. Chronic GVHD and pretransplantation abnormalities in pulmonary function are the main determinants predicting worsening pulmonary function in long-term survivors after stem cell transplantation. Biol Blood Marrow Transplant 2006; 12: 1261–1269.
Nishio N, Yagasaki H, Takahashi Y, Muramatsu H, Hama A, Tanaka M et al. Late-onset non-infectious pulmonary complications following allogeneic hematopoietic stem cell transplantation in children. Bone Marrow Transplant 2009; 44: 303–308.
Freudenberger TD, Madtes DK, Curtis JR, Cummings P, Storer BE, Hackman RC . Association between acute and chronic graft-versus-host disease and bronchiolitis obliterans organizing pneumonia in recipients of hematopoietic stem cell transplants. Blood 2003; 102: 3822–3828.
Uderzo C, Pillon M, Corti P, Tridello G, Tana F, Zintl F et al. Impact of cumulative anthracycline dose, preparative regimen and chronic graft-versus-host disease on pulmonary and cardiac function in children 5 years after allogeneic hematopoietic stem cell transplantation: a prospective evaluation on behalf of the EBMT Pediatric Diseases and Late Effects Working Parties. Bone Marrow Transplant 2007; 39: 667–675.
Filipovich AH, Weisdorf D, Pavletic S, Socie G, Wingard JR, Lee SJ et al. National Institutes of Health consensus development project on criteria for clinical trials in chronic graft-versus-host disease: I. Diagnosis and staging working group report. Biol Blood Marrow Transplant 2005; 11: 945–956.
Williams KM, Chien JW, Gladwin MT, Pavletic SZ . Bronchiolitis obliterans after allogeneic hematopoietic stem cell transplantation. JAMA 2009; 302: 306–314.
Couriel D, Carpenter PA, Cutler C, Bolanos-Meade J, Treister NS, Gea-Banacloche J et al. Ancillary therapy and supportive care of chronic graft-versus-host disease: national institutes of health consensus development project on criteria for clinical trials in chronic Graft-versus-host disease: V. Ancillary Therapy and Supportive Care Working Group Report. Biol Blood Marrow Transplant 2006; 12: 375–396.
Clark JG, Crawford SW, Madtes DK, Sullivan KM . Obstructive lung disease after allogeneic marrow transplantation. Clinical presentation and course. Ann Intern Med 1989; 111: 368–376.
Sullivan K, Mori M, Sanders J, Siadak M, Witherspoon RP, Anasetti C et al. Late complications of allogeneic and autologous bone marrow transplantation. Bone Marrow Transplant 1992; 10: 127–134.
Sanchez J, Torres A, Serrano J, Romain J, Martin C, Perula L et al. Long term follow up of immunosuppressive treatment for obstructive airway disease after allogeneic bone marrow transplantation. Bone Marrow Transplant 1997; 20: 403–408.
Badier M, Guillot C, Delpierre S, Vanuxem P, Blaise D, Maraninchi D . Pulmonary function changes 100 days and one year after bone marrow transplantation. Bone Marrow Transplant 1993; 12: 457–461.
Crawford SW, Pepe M, Lin D, Benedetti F, Deeg HJ . Abnormalities of pulmonary function tests after marrow transplantation predict nonrelapse mortality. Am J Respir Crit Care Med 1995; 152: 690–695.
Watkins TR, Chien JW, Crawford SW . Graft versus host-associated pulmonary disease and other idiopathic pulmonary complications after hematopoietic stem cell transplant. Semin Respir Crit Care Med 2005; 26: 482–489.
Chien JW, Martin PJ, Gooley TA, Flowers ME, Heckbert SR, Nichols WG et al. Airflow obstruction after myeloablative allogeneic hematopoietic stem cell transplantation. Am J Respir Crit Care Med 2003; 168: 208–214.
Afessa B, Litzow MR, Tefferi A . Bronchiolitis obliterans and other late onset non-infectious pulmonary complications in hematopoietic stem cell transplantation. Bone Marrow Transplant 2001; 28: 425–434.
Holland HK, Wingard JR, Beschorner WE, Saral R, Santos GW . Bronchiolitis obliterans in bone marrow transplantation and its relationship to chronic graft-versus-host disease and low serum IgG. Blood 1988; 72: 621–627.
Palmas A, Tefferi A, Myers JL, Scott JP, Swensen SJ, Chen MG et al. Late-onset noninfectious pulmonary complications after allogeneic bone marrow transplantation. Br J Haematol 1998; 100: 680–687.
Duncker C, Dohr D, Harsdorf S, Duyster J, Stefanic M, Martini C et al. Non-infectious lung complications are closely associated with chronic graft-versus-host disease: a single center study of incidence, risk factors and outcome. Bone Marrow Transplant 2000; 25: 1263–1268.
Marras TK, Chan CK, Lipton JH, Messner HA, Szalai JP, Laupacis A . Long-term pulmonary function abnormalities and survival after allogeneic marrow transplantation. Bone Marrow Transplant 2004; 33: 509–517.
Jacobsohn DA, Schechter T, Seshadri R, Thormann K, Duerst R, Kletzel M . Eosinophilia correlates with the presence or development of chronic graft-versus-host disease in children. Transplantation 2004; 77: 1096–1100.
ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med 2002; 166: 111–117.
Chien JW, Madtes DK, Clark JG . Pulmonary function testing prior to hematopoietic stem cell transplantation. Bone Marrow Transplant 2005; 35: 429–435.
Efrati O, Toren A, Duskin H, Modan-Moses D, Bielorai B, Goldstein G et al. Pulmonary function studies in children treated by chemoradiotherapy and stem cell transplantation. Pediatr Blood Cancer 2008; 51: 684–688.
Walter EC, Orozco-Levi M, Ramirez-Sarmiento A, Vigorito A, Campregher PV, Martin PJ et al. Lung function and long-term complications after allogeneic hematopoietic cell transplant. Biol Blood Marrow Transplant 2010; 16: 53–61.
Wolff D, Herzberg P, Heussner P, Mumm F, Hilgendorf I, von Harsdorf S et al. Chronic GVHD of the lung significantly impairs quality of life and the activity profile—Results of a prospective German multicenter validation trial. Bone Marrow Transplant 2009; 43: P541.
Rabanus R, Hahn J, Andreesen R, Holler E, Hildebrandt GC . Risk factor analysis for the development of restrictive and obstructive pulmonary function changes after allogeneic stem cell transplantation. Biol Blood Marrow Transpl 2008; 14: S6.
Pellegrino R, Viegi G, Brusasco V, Crapo RO, Burgos F, Casaburi R et al. Interpretative strategies for lung function tests. Eur Respir J 2005; 26: 948–968.
Yokoi T, Hirabayashi N, Ito M, Uno Y, Tsuzuki T, Yatabe Y et al. Broncho-bronchiolitis obliterans as a complication of bone marrow transplantation: a clinicopathological study of eight autopsy cases. Nagoya BMT Group Virchows Arch 1997; 431: 275–282.
Vogelsang GB, Lee L, Bensen-Kennedy DM . Pathogenesis and treatment of graft-versus-host disease after bone marrow transplant. Annu Rev Med 2003; 54: 29–52.
Miller MR, Crapo R, Hankinson J, Brusasco V, Burgos F, Casaburi R et al. General considerations for lung function testing. Eur Respir J 2005; 26: 153–161.
Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A et al. Standardisation of spirometry. Eur Respir J 2005; 26: 319–338.
Marras TK, Szalai JP, Chan CK, Lipton JH, Messner HA, Laupacis A . Pulmonary function abnormalities after allogeneic marrow transplantation: a systematic review and assessment of an existing predictive instrument. Bone Marrow Transplant 2002; 30: 599–607.
Chiou TJ, Tung SL, Wang WS, Tzeng WF, Yen CC, Fan FS et al. Pulmonary function changes in long-term survivors of chronic myelogenous leukemia after allogeneic bone marrow transplantation: a Taiwan experience. Cancer Invest 2002; 20: 880–888.
Ghalie R, Szidon JP, Thompson L, Nawas YN, Dolce A, Kaizer H . Evaluation of pulmonary complications after bone marrow transplantation: the role of pretransplant pulmonary function tests. Bone Marrow Transplant 1992; 10: 359–365.
Crawford SW, Fisher L . Predictive value of pulmonary function tests before marrow transplantation. Chest 1992; 101: 1257–1264.
Pavletic SZ, Martin P, Lee SJ, Mitchell S, Jacobsohn D, Cowen EW et al. Measuring therapeutic response in chronic graft-versus-host disease: National Institute of Health Consensus Development Project on criteria for clinical trials in chronic graft-versus-host disease: IV.Response criteria working group report. Biol Blood Marrow Transpl 2006; 12: 252–266.
Parimon T, Madtes DK, Au DH, Clark JG, Chien JW . Pretransplant lung function, respiratory failure, and mortality after stem cell transplantation. Am J Respir Crit Care Med 2005; 172: 384–390.
Kanamori H, Fujisawa S, Tsuburai T, Yamaji S, Tomita N, Fujimaki K et al. Increased exhaled nitric oxide in bronchiolitis obliterans organizing pneumonia after allogeneic bone marrow transplantation. Transplantation 2002; 74: 1356–1358.
Worthy SA, Flint JD, Muller NL . Pulmonary complications after bone marrow transplantation: high-resolution CT and pathologic findings. Radiographics 1997; 17: 1359–1371.
Gunn ML, Godwin JD, Kanne JP, Flowers ME, Chien JW . High-resolution CT findings of bronchiolitis obliterans syndrome after hematopoietic stem cell transplantation. J Thorac Imaging 2008; 23: 244–250.
Escuissato DL, Gasparetto EL, Marchiori E, Rocha Gde M, Inoue C, Pasquini R et al. Pulmonary infections after bone marrow transplantation: high-resolution CT findings in 111 patients. AJR Am J Roentgenol 2005; 185: 608–615.
Gasparetto TD, Escuissato DL, Marchiori E . Pulmonary infections following bone marrow transplantation: high-resolution CT findings in 35 paediatric patients. Eur J Radiol 2008; 66: 117–121.
Rochat I, Posfay-Barbe KM, Kumar N, Pache JC, Kaiser L, Ozsahin H et al. Bronchoalveolar cytology for diagnosing pulmonary GVHD after bone marrow transplant in children. Pediatr Pulmonol 2008; 43: 697–702.
Kasow KA, King E, Rochester R, Tong X, Srivastava DK, Horwitz EM et al. Diagnostic yield of bronchoalveolar lavage is low in allogeneic hematopoietic stem cell recipients receiving immunosuppressive therapy or with acute graft-versus-host disease: the St. Jude experience, 1990-2002. Biol Blood Marrow Transplant 2007; 13: 831–837.
Chamberlain D, Maurer J, Chaparro C, Idolor L . Evaluation of transbronchial lung biopsy specimens in the diagnosis of bronchiolitis obliterans after lung transplantation. J Heart Lung Transplant 1994; 13: 963–971.
Hayes-Jordan A, Benaim E, Richardson S, Joglar J, Srivastava DK, Bowman L et al. Open lung biopsy in pediatric bone marrow transplant patients. J Pediatr Surg 2002; 37: 446–452.
White DA, Wong PW, Downey R . The utility of open lung biopsy in patients with hematologic malignancies. Am J Respir Crit Care Med 2000; 161 (3 Part 1): 723–729.
Gower WA, Collaco JM, Mogayzel Jr PJ . Pulmonary dysfunction in pediatric hematopoietic stem cell transplant patients: non-infectious and long-term complications. Pediatr Blood Cancer 2007; 49: 225–233.
Chien JW, Duncan S, Williams KM, Pavletic SZ . Bronchiolitis obliterans syndrome after allogeneic hematopoetic stem cell transplantation—an increasingly recognized manifestation of chronic graft-versus-host-disease. Biol Blood Marrow Transplant 2010; 16: S106–S114.
Yousem SA . The histological spectrum of pulmonary graft-versus-host disease in bone marrow transplant recipients. Hum Pathol 1995; 26: 668–675.
Bergeron A, Belle A, Chevret S, Ribaud P, Devergie A, Esperou H et al. Combined inhaled steroids and bronchodilatators in obstructive airway disease after allogeneic stem cell transplantation. Bone Marrow Transplant 2007; 39: 547–553.
Bergeron A, Chagnon K, Feuillet S, Chevret S, Tazi A . Prospective evaluation of the efficacy of the combination of budesonide/formoterol in obstructive airway disease after allogeneic hematopoietic stem cell transplantation]. Revue Des Maladies Respiratoires 2009; 26: 794–800.
Bashoura L, Gupta S, Jain A, Couriel DR, Komanduri KV, Eapen GA et al. Inhaled corticosteroids stabilize constrictive bronchiolitis after hematopoietic stem cell transplantation. Bone Marrow Transplant 2008; 41: 63–67.
Hendriks T, de Hoog M, Lequin MH, Devos AS, Merkus PJ . DNase and atelectasis in non-cystic fibrosis pediatric patients. Crit Care 2005; 9: R351–R356.
Rimensberger PC, Spahr-Schopfer I, Berner M, Jaeggi E, Kalangos A, Friedli B et al. Inhaled nitric oxide versus aerosolized iloprost in secondary pulmonary hypertension in children with congenital heart disease: vasodilator capacity and cellular mechanisms. Circulation 2001; 103: 544–548.
Ivy DD, Doran AK, Smith KJ, Mallory Jr GB, Beghetti M, Barst RJ et al. Short- and long-term effects of inhaled iloprost therapy in children with pulmonary arterial hypertension. J Am Coll Cardiol 2008; 51: 161–169.
Dudek AZ, Mahaseth H, DeFor TE, Weisdorf DJ . Bronchiolitis obliterans in chronic graft-versus-host disease: analysis of risk factors and treatment outcomes. Biol Blood Marrow Transplant 2003; 9: 657–666.
Duncan CN, Buonanno MR, Barry EV, Myers K, Peritz D, Lehmann L . Bronchiolitis obliterans following pediatric allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplant 2008; 41: 971–975.
Ratjen F, Rjabko O, Kremens B . High-dose corticosteroid therapy for bronchiolitis obliterans after bone marrow transplantation in children. Bone Marrow Transplant 2005; 36: 135–138.
Smith EP, Sniecinski I, Dagis AC, Parker PM, Snyder DS, Stein AS et al. Extracorporeal photochemotherapy for treatment of drug-resistant graft-vs host disease. Biol Blood Marrow Transplant 1998; 4: 27–37.
Garban F, Drillat P, Makowski C, Jacob MC, Richard MJ, Favrot M et al. Extracorporeal chemophototherapy for the treatment of graft-versus-host disease: hematologic consequences of short-term, intensive courses. Haematologica 2005; 90: 1096–1101.
Couriel DR, Hosing C, Saliba R, Shpall EJ, Anderlini P, Rhodes B et al. Extracorporeal photochemotherapy for the treatment of steroid-resistant chronic GVHD. Blood 2006; 107: 3074–3080.
Ilhan O, Arat M, Arslan O, Ayyildiz E, Sanli H, Beksac M et al. Extracorporeal photoimmunotherapy for the treatment of steroid refractory progressive chronic graft-versus-host disease. Transfus Apher Sci 2004; 30: 185–187.
Oyan B, Koc Y, Emri S, Kansu E . Improvement of chronic pulmonary graft-vs-host disease manifesting as bronchiolitis obliterans organizing pneumonia following extracorporeal photopheresis. Med Oncol 2006; 23: 125–129.
Couriel D, Hosing C, Saliba R, Shpall EJ, Andelini P, Popat U et al. Extracorporeal photopheresis for acute and chronic graft-versus-host disease: does it work? Biol Blood Marrow Transplant 2006; 12 (1 Suppl 2): 37–40.
Child FJ, Ratnavel R, Watkins P, Samson D, Apperley J, Ball J et al. Extracorporeal photopheresis (ECP) in the treatment of chronic graft-versus-host disease (GVHD). Bone Marrow Transplant 1999; 23: 881–887.
Lucid CE, Savani BN, Engelhardt BG, Shah P, Clifton C, Greenhut SL et al. Extracorporeal photopheresis in patients with refractory bronchiolitis obliterans developing after allo-SCT. Bone Marrow Transplant 2011; 46: 426–429.
Groetzner J, Wittwer T, Kaczmarek I, Ueberfuhr P, Strauch J, Nagib R et al. Conversion to sirolimus and mycophenolate can attenuate the progression of bronchiolitis obliterans syndrome and improves renal function after lung transplantation. Transplantation 2006; 81: 355–360.
Hernandez RL, Gil PU, Gallo CG, de Pablo Gafas A, Hernandez MC, Alvarez MJ . Rapamycin in lung transplantation. Transplant Proc 2005; 37: 3999–4000.
Snell GI, Valentine VG, Vitulo P, Glanville AR, McGiffin DC, Loyd JE et al. Everolimus versus azathioprine in maintenance lung transplant recipients: an international, randomized, double-blind clinical trial. Am J Transplant 2006; 6: 169–177.
Borro JM, Bravo C, Sole A, Usetti P, Zurbano F, Lama R et al. Conversion from cyclosporine to tacrolimus stabilizes the course of lung function in lung transplant recipients with bronchiolitis obliterans syndrome. Transplant Proc 2007; 39: 2416–2419.
Celik MR, Lederer DJ, Wilt J, Eser D, Bacchetta M, D’Ovidio F et al. Tacrolimus and azathioprine versus cyclosporine and mycophenolate mofetil after lung transplantation: a retrospective cohort study. J Heart Lung Transplant 2009; 28: 697–703.
Wolff D, Gerbitz A, Ayuk F, Kiani A, Hildebrandt GC, Vogelsang GB et al. Consensus conference on clinical practice in chronic graft-versus-host disease (GVHD): first-line and topical treatment of chronic GVHD. Biol Blood Marrow Transplant 2010; 16: 1611–1628.
Wolff D, Schleuning M, von Harsdorf S, Bacher U, Gerbitz A, Stadler M et al. Consensus conference on clinical practice in chronic GVHD: second-line treatment of chronic graft-versus-host disease. Biol Blood Marrow Transplant 2011; 17: 1–17.
Gerhardt SG, McDyer JF, Girgis RE, Conte JV, Yang SC, Orens JB . Maintenance azithromycin therapy for bronchiolitis obliterans syndrome: results of a pilot study. Am J Respir Crit Care Med 2003; 168: 121–125.
Verleden GM, Dupont LJ . Azithromycin therapy for patients with bronchiolitis obliterans syndrome after lung transplantation. Transplantation 2004; 77: 1465–1467.
Gottlieb J, Szangolies J, Koehnlein T, Golpon H, Simon A, Welte T . Long-term azithromycin for bronchiolitis obliterans syndrome after lung transplantation. Transplantation 2008; 85: 36–41.
Khalid M, Al Saghir A, Saleemi S, Al Dammas S, Zeitouni M, Al Mobeireek A et al. Azithromycin in bronchiolitis obliterans complicating bone marrow transplantation: a preliminary study. Eur Respir J 2005; 25: 490–493.
Verleden GM, Vanaudenaerde BM, Dupont LJ, Van Raemdonck DE . Azithromycin reduces airway neutrophilia and interleukin-8 in patients with bronchiolitis obliterans syndrome. Am J Respir Crit Care Med 2006; 174: 566–570.
Mertens V, Blondeau K, Pauwels A, Farre R, Vanaudenaerde B, Vos R et al. Azithromycin reduces gastroesophageal reflux and aspiration in lung transplant recipients. Dig Dis Sci 2009; 54: 972–979.
King BJ, Iyer H, Leidi AA, Carby MR . Gastroesophageal reflux in bronchiolitis obliterans syndrome: a new perspective. J Heart Lung Transplant 2009; 28: 870–875.
Vanaudenaerde BM, Meyts I, Vos R, Geudens N, De Wever W, Verbeken EK et al. A dichotomy in bronchiolitis obliterans syndrome after lung transplantation revealed by azithromycin therapy. Eur Respir J 2008; 32: 832–843.
St John RC, Gadek JE, Tutschka PJ, Kapoor N, Dorinsky PM . Analysis of airflow obstruction by bronchoalveolar lavage following bone marrow transplantation. Implications for pathogenesis and treatment. Chest 1990; 98: 600–607.
Yanik GA, Ho VT, Levine JE, White ES, Braun T, Antin JH et al. The impact of soluble tumor necrosis factor receptor etanercept on the treatment of idiopathic pneumonia syndrome after allogeneic hematopoietic stem cell transplantation. Blood 2008; 112: 3073–3081.
Fullmer JJ, Fan LL, Dishop MK, Rodgers C, Krance R . Successful treatment of bronchiolitis obliterans in a bone marrow transplant patient with tumor necrosis factor-alpha blockade. Pediatrics 2005; 116: 767–770.
Tun HW, Wallace KH, Grinton SF, Khoor A, Burger CD . Etanercept therapy for late-onset idiopathic pneumonia syndrome after nonmyeloablative allogeneic hematopoietic stem cell transplantation. Transplant Proc 2005; 37: 4492–4496.
Ramirez AM, Takagawa S, Sekosan M, Jaffe HA, Varga J, Roman J . Smad3 deficiency ameliorates experimental obliterative bronchiolitis in a heterotopic tracheal transplantation model. Am J Pathol 2004; 165: 1223–1232.
Hertz MI, Henke CA, Nakhleh RE, Harmon KR, Marinelli WA, Fox JM et al. Obliterative bronchiolitis after lung transplantation: a fibroproliferative disorder associated with platelet-derived growth factor. Proc Natl Acad Sci USA 1992; 89: 10385–10389.
Svegliati S, Olivieri A, Campelli N, Luchetti M, Poloni A, Trappolini S et al. Stimulatory autoantibodies to PDGF receptor in patients with extensive chronic graft-versus-host disease. Blood 2007; 110: 237–241.
McCormick LL, Zhang Y, Tootell E, Gilliam AC . Anti-TGF-beta treatment prevents skin and lung fibrosis in murine sclerodermatous graft-versus-host disease: a model for human scleroderma. J Immunol 1999; 163: 5693–5699.
Majhail NS, Schiffer CA, Weisdorf DJ . Improvement of pulmonary function with imatinib mesylate in bronchiolitis obliterans following allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transplant 2006; 12: 789–791.
Olivieri A, Locatelli F, Zecca M, Sanna A, Cimminiello M, Raimondi R et al. Imatinib for refractory chronic graft-versus-host disease with fibrotic features. Blood 2009; 114: 709–718.
Daniels CE, Wilkes MC, Edens M, Kottom TJ, Murphy SJ, Limper AH et al. Imatinib mesylate inhibits the profibrogenic activity of TGF-beta and prevents bleomycin-mediated lung fibrosis. J Clin Invest 2004; 114: 1308–1316.
Aono Y, Nishioka Y, Inayama M, Ugai M, Kishi J, Uehara H et al. Imatinib as a novel antifibrotic agent in bleomycin-induced pulmonary fibrosis in mice. Am J Respir Crit Care Med 2005; 171: 1279–1285.
Distler JH, Jungel A, Huber LC, Schulze-Horsel U, Zwerina J, Gay RE et al. Imatinib mesylate reduces production of extracellular matrix and prevents development of experimental dermal fibrosis. Arthritis Rheum 2007; 56: 311–322.
Wilborn J, Bailie M, Coffey M, Burdick M, Strieter R, Peters-Golden M . Constitutive activation of 5-lipoxygenase in the lungs of patients with idiopathic pulmonary fibrosis. J Clin Invest 1996; 97: 1827–1836.
Medoff BD, Seung E, Wain JC, Means TK, Campanella GS, Islam SA et al. BLT1-mediated T cell trafficking is critical for rejection and obliterative bronchiolitis after lung transplantation. J Exp Med 2005; 202: 97–110.
Peters-Golden M . Expanding roles for leukotrienes in airway inflammation. Curr Allergy Asthma Rep 2008; 8: 367–373.
Peters-Golden M, Bailie M, Marshall T, Wilke C, Phan SH, Toews GB et al. Protection from pulmonary fibrosis in leukotriene-deficient mice. Am J Respir Crit Care Med 2002; 165: 229–235.
Simms RW, Korn JH . The role of leukotrienes in alveolitis associated with scleroderma. Arthritis Rheum 2003; 48: 1478–1480.
Or R, Gesundheit B, Resnick I, Bitan M, Avraham A, Avgil M et al. Sparing effect by montelukast treatment for chronic graft versus host disease: a pilot study. Transplantation 2007; 83: 577–581.
Norman BC, Jacobsohn D, Williams KM, Au B, Au MA, Lee SJ et al. Fluticasone, azithromycin, and montelukast (FAM) therapy in reducing steroid exposure ni bronchiolitis obliterans syndrome after allogeneic hematopoetic stem cell transplant (HCT)—a case series of 8 patients. Biol Blood Marrow Transplant 2010; 16: S308.
Waer M, Vanrenterghem Y, Roels L, Verberckmoes R, Hauglustaine D, van der Schueren E et al. Renal cadaveric transplantation in diabetics using total lymphoid irradiation or cyclosporin A. A controlled randomized study Leuven Collaborative Transplantation Group. Transpl Int 1988; 1: 64–68.
Lim TS, O′Driscoll G, Freund J, Peterson V, Hayes H, Heywood J . Short-course total lymphoid irradiation for refractory cardiac transplantation rejection. J Heart Lung Transplant 2007; 26: 1249–1254.
Asano M, Gundry SR, Razzouk AJ, del Rio MJ, Thomas M, Chinnock RE et al. Total lymphoid irradiation for refractory rejection in pediatric heart transplantation. Ann Thorac Surg 2002; 74: 1979–1985.
Fisher AJ, Rutherford RM, Bozzino J, Parry G, Dark JH, Corris PA . The safety and efficacy of total lymphoid irradiation in progressive bronchiolitis obliterans syndrome after lung transplantation. Am J Transplant 2005; 5: 537–543.
Iacono AT, Johnson BA, Grgurich WF, Youssef JG, Corcoran TE, Seiler DA et al. A randomized trial of inhaled cyclosporine in lung-transplant recipients. N Engl J Med 2006; 354: 141–150.
Iacono AT, Corcoran TE, Griffith BP, Grgurich WF, Smith DA, Zeevi A et al. Aerosol cyclosporin therapy in lung transplant recipients with bronchiolitis obliterans. Eur Respir J 2004; 23: 384–390.
Behr J, Zimmermann G, Baumgartner R, Leuchte H, Neurohr C, Brand P et al. Lung deposition of a liposomal cyclosporine A inhalation solution in patients after lung transplantation. J Aerosol Med Pulm Drug Deliv 2009; 22: 121–130.
Svendsen UG, Aggestrup S, Heilmann C, Jacobsen N, Koch C, Larsen B et al. Transplantation of a lobe of lung from mother to child following previous transplantation with maternal bone marrow. Eur Respir J 1995; 8: 334–337.
Heath JA, Kurland G, Spray TL, Kernan NA, Small TN, Brochstein JA et al. Lung transplantation after allogeneic marrow transplantation in pediatric patients: the Memorial Sloan-Kettering experience. Transplantation 2001; 72: 1986–1990.
Rabitsch W, Deviatko E, Keil F, Herold C, Dekan G, Greinix HT et al. Successful lung transplantation for bronchiolitis obliterans after allogeneic marrow transplantation. Transplantation 2001; 71: 1341–1343.
Calhoon JH, Levine S, Anzueto A, Bryan CL, Trinkle JK . Lung transplantation in a patient with a prior bone marrow transplant. Chest 1992; 102: 948.
Boas SR, Noyes BE, Kurland G, Armitage J, Orenstein D . Pediatric lung transplantation for graft-versus-host disease following bone marrow transplantation. Chest 1994; 105: 1584–1586.
Sano Y, Date H, Nagahiro I, Aoe M, Shimizu N . Living-donor lobar lung transplantation for bronchiolitis obliterans after bone marrow transplantation. Ann Thorac Surg 2005; 79: 1051–1052.
Panoskaltsis-Mortari A, Tram KV, Price AP, Wendt CH, Blazar BR . A new murine model for bronchiolitis obliterans post-bone marrow transplant. Am J Respir Crit Care Med 2007; 176: 713–723.
Acknowledgements
We thank all participating centers of conferences and surveys, which included participants from the transplant centers in Augsburg, Basel, Berlin, Cologne, Dresden, Duesseldorf, Erlangen, Essen, Freiburg, Greifswald, Hamburg, Hannover, Heidelberg, Jena, Kiel, Leipzig, Linz, Mainz, Münster, Munich, Nantes, Nuernberg, Oldenburg, Paris, Regensburg, Rostock, Tuebingen, Ulm, Vienna, Wiesbaden and Wuerzburg. We thank Anna Hackl for evaluating the survey on treatment of cGVHD. The conference was supported by the Jose Carreras Foundation project ‘Competence center GVHD Regensburg’. We convey our special thanks to Dr Nicolai Kittan for his critical review of the manuscript and figure design.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Hildegard Greinix served as member of a steering committee for a chronic GVHD study of Therakos and received honoraria from Therakos for research presentations in corporate symposia at international scientific meetings. The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Hildebrandt, G., Fazekas, T., Lawitschka, A. et al. Diagnosis and treatment of pulmonary chronic GVHD: report from the consensus conference on clinical practice in chronic GVHD. Bone Marrow Transplant 46, 1283–1295 (2011). https://doi.org/10.1038/bmt.2011.35
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2011.35
Keywords
This article is cited by
-
Clinical risk factors and prognostic model for patients with bronchiolitis obliterans syndrome after hematopoietic stem cell transplantation
Bone Marrow Transplantation (2024)
-
Graft-Versus-Host Disease: an Update on Functional Implications and Rehabilitation Interventions
Current Oncology Reports (2023)
-
Association between early corticosteroid administration and long-term survival in non-infectious pulmonary complications after allogeneic hematopoietic stem cell transplantation
International Journal of Hematology (2023)
-
The predictive value of pulmonary function test before transplantation for chronic pulmonary graft-versus-host-disease after allogeneic hematopoietic stem cell transplantation
BMC Pulmonary Medicine (2022)
-
Longitudinal lung function in childhood cancer survivors after hematopoietic stem cell transplantation
Bone Marrow Transplantation (2022)