Abstract
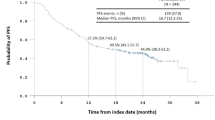
Primary pulmonary MALT lymphoma is a rare disease, and no standard treatments have been defined yet. In this study, 38 consecutive patients from single center were reviewed. Among 25 patients with localized disease, radical surgery were performed in 12 patients, and the other 13 patients had chemotherapy combined with (7 patients) or without (6 patients) radiotherapy. No significant difference in overall survival (OS) was found between patients who received surgery or not; however, patients treated with chemotherapy had superior progression-free survival (PFS) than those treated with upfront surgery (P = 0.032). Among the 12 patients who received radical surgery, 7 were given adjuvant chemotherapy and 1 patient had consolidation radiotherapy. No significant differences in PFS and OS exist between those who received adjuvant treatment or not (P > 0.05). For patients who received chemotherapy, PFS and OS were significantly better for those treated with cyclophosphamide-based therapy than fludarabine-based therapy. At a median follow-up time of 61.1 months, 5- and 10-year PFS rate was 70.0 and 43.0 %, respectively, and 5- and 10-year OS rate was both 81.0 %. In conclusion, we confirmed the indolent behavior and favorable outcome of this disease. In order to preserve lung function and reduce the risks associated with surgery, radiotherapy or rituximab in combination with alkylating drug-based chemotherapy should be considered as first-line option for pulmonary MALT lymphoma.




Similar content being viewed by others
References
A clinical evaluation of the International Lymphoma Study Group classification of non-Hodgkin’s lymphoma. The non-Hodgkin’s Lymphoma Classification Project. Blood 1997;89:3909–3918.
Radaszkiewicz T, Dragosics B, Bauer P. Gastrointestinal malignant lymphomas of the mucosa-associated lymphoid tissue: factors relevant to prognosis. Gastroenterology. 1992;102:1628–38.
Thieblemont C, Berger F, Dumontet C, Moullet I, Bouafia F, Felman P, et al. Mucosa-associated lymphoid tissue lymphoma is a disseminated disease in one third of 158 patients analyzed. Blood. 2000;95:802–6.
Isaacson P, Wright DH. Extranodal malignant lymphoma arising from mucosa-associated lymphoid tissue. Cancer. 1984;53:2515–24.
Suarez F, Lortholary O, Hermine O, Lecuit M. Infection-associated lymphomas derived from marginal zone B cells: a model of antigen-driven lymphoproliferation. Blood. 2006;107:3034–44.
Royer B, Cazals-Hatem D, Sibilia J, Agbalika F, Cayuela JM, Soussi T, et al. Lymphomas in patients with Sjogren’s syndrome are marginal zone B-cell neoplasms, arise in diverse extranodal and nodal sites, and are not associated with viruses. Blood. 1997;90:766–75.
Wotherspoon AC, Doglioni C, Diss TC, Pan L, Moschini A, de Boni M, et al. Regression of primary low-grade B-cell gastric lymphoma of mucosa-associated lymphoid tissue type after eradication of Helicobacter pylori. Lancet. 1993;342:575–7.
Tschernig T, Pabst R. Bronchus-associated lymphoid tissue (BALT) is not present in the normal adult lung but in different diseases. Pathobiol: J Immunopathol Mol Cell Biol. 2000;68:1–8.
Savio A, Franzin G, Wotherspoon AC, Zamboni G, Negrini R, Buffoli F, et al. Diagnosis and posttreatment follow-up of Helicobacter pylori-positive gastric lymphoma of mucosa-associated lymphoid tissue: histology, polymerase chain reaction, or both? Blood. 1996;87:1255–60.
Stefanovic A, Morgensztern D, Fong T, Lossos IS. Pulmonary marginal zone lymphoma: a single centre experience and review of the SEER database. Leuk Lymphoma. 2008;49:1311–20.
Troch M, Streubel B, Petkov V, Turetschek K, Chott A, Raderer M. Does MALT lymphoma of the lung require immediate treatment? An analysis of 11 untreated cases with long-term follow-up. Anticancer Res. 2007;27:3633–7.
Oh SY, Ryoo BY, Kim WS, Park YH, Kim K, Kim HJ, et al. Nongastric marginal zone B-cell lymphoma: analysis of 247 cases. Am J Hematol. 2007;82:446–52.
Kim JH, Lee SH, Park J, Kim HY, Lee SI, Park JO, et al. Primary pulmonary non-Hodgkin’s lymphoma. Jpn J Clin Oncol. 2004;34:510–4.
Chanudet E, Adam P, Nicholson AG, Wotherspoon AC, Ranaldi R, Goteri G, et al. Chlamydiae and Mycoplasma infections in pulmonary MALT lymphoma. Br J Cancer. 2007;97:949–51.
Oh SY, Kim WS, Kim JS, Kim SJ, Kwon HC, Lee DH, et al. Pulmonary marginal zone B-cell lymphoma of MALT type—what is a prognostic factor and which is the optimal treatment, operation, or chemotherapy?: Consortium for Improving Survival of Lymphoma (CISL) study. Ann Hematol. 2010;89:563–8.
Liang Y, Wang L, Zhu Y, Lin Y, Liu H, Rao H, et al. Primary pulmonary lymphoepithelioma-like carcinoma: fifty-two patients with long-term follow-up. Cancer. 2012;118:4748–58.
Rosebeck S, Rehman AO, Apel IJ, Kohrt D, Appert A, O’Donnell MA, et al. The API2-MALT1 fusion exploits TNFR pathway-associated RIP1 ubiquitination to promote oncogenic NF-kappab signaling. Oncogene. 2014;33:2520–30.
Tsai AG, Lu Z, Lieber MR. The t(14;18)(q32;q21)/IGH-MALT1 translocation in MALT lymphomas is a CpG-type translocation, but the t(11;18)(q21;q21)/API2-MALT1 translocation in MALT lymphomas is not. Blood. 2010;115:3640–1. author reply 3641–3642.
Xia H, Nakayama T, Sakuma H, Yamada S, Sato F, Takino H, et al. Analysis of API2-MALT1 fusion, trisomies, and immunoglobulin VH genes in pulmonary mucosa-associated lymphoid tissue lymphoma. Hum Pathol. 2011;42:1297–304.
Borie R, Wislez M, Thabut G, Antoine M, Rabbat A, Couderc LJ, et al. Clinical characteristics and prognostic factors of pulmonary malt lymphoma. Eur Respir J. 2009;34:1408–16.
Li AW, Xu JF, Zhou CC, Wu CY, Wang YL. Clinical characteristics and diagnosis of pulmonary mucosa-associated lymphoid tissue-derived (MALT) lymphoma: a retrospective analysis of 29 cases. Zhonghua Zhong Liu Za Zhi Chin J Oncol. 2012;34:390–3.
Solal-Celigny P, Bellei M, Marcheselli L, Pesce EA, Pileri S, McLaughlin P, et al. Watchful waiting in low-tumor burden follicular lymphoma in the rituximab era: results of an F2-study database. J Clin Oncol: Off J Am Soc Clin Oncol. 2012;30:3848–53.
Wirth A, Gospodarowicz M, Aleman BM, Bressel M, Ng A, Chao M, et al. Long-term outcome for gastric marginal zone lymphoma treated with radiotherapy: a retrospective, multi-centre, International Extranodal Lymphoma Study Group study. Ann Oncol: Off J Eur Soc Med Oncol ESMO. 2013;24:1344–51.
Olszewski AJ, Castillo JJ. Comparative outcomes of oncologic therapy in gastric extranodal marginal zone (MALT) lymphoma: analysis of the SEER-Medicare database. Ann Oncol: Off J Eur Soc Med Oncol ESMO. 2013;24:1352–9.
Harada K, Murakami N, Kitaguchi M, Sekii S, Takahashi K, Yoshio K, et al. Localized ocular adnexal mucosa-associated lymphoid tissue lymphoma treated with radiation therapy: a long-term outcome in 86 patients with 104 treated eyes. Int J Radiat Oncol Biol Phys. 2014;88:650–4.
Chong EA, Svoboda J, Cherian S, Andreadis C, Downs LH, Zhuang H, et al. Regression of pulmonary MALT lymphoma after treatment with rituximab. Leuk Lymphoma. 2005;46:1383–6.
Yoshida C, Tarumi S, Kato A, Nii K, Chang SS, Yokomise H. Mucosa-associated lymphoid tissue (MALT) lymphoma of the lung treated by surgery and rituximab; report of a case. Kyobu Geka Jpn J Thorac Surg. 2013;66:169–72.
Zucca E, Conconi A, Laszlo D, Lopez-Guillermo A, Bouabdallah R, Coiffier B, et al. Addition of rituximab to chlorambucil produces superior event-free survival in the treatment of patients with extranodal marginal-zone b-cell lymphoma: 5-year analysis of the IELSG-19 Randomized Study. J Clin Oncol: Off J Am Soc Clin Oncol. 2013;31:565–72.
Troch M, Jonak C, Mullauer L, Puspok A, Formanek M, Hauff W, et al. A phase II study of bortezomib in patients with MALT lymphoma. Haematologica. 2009;94:738–42.
Conconi A, Martinelli G, Lopez-Guillermo A, Zinzani PL, Ferreri AJ, Rigacci L, et al. Clinical activity of bortezomib in relapsed/refractory MALT lymphomas: results of a phase II study of the International Extranodal Lymphoma Study Group (IELSG). Ann Oncol: Off J Eur Soc Med Oncol ESMO. 2011;22:689–95.
Acknowledgments
We thank all physicians at Sun Yat-sen University Cancer Center for allowing us to include their patients. We also appreciate the cooperation of all pathologists at Sun Yat-sen University Cancer Center for their support. This work received grant support from the National Natural Science Foundation of China (contract/grant number: 81400159), the Medical Research Foundation of Guangdong Province (grant number: B2014158), the Young Teachers’ Cultivation Project of Sun Yat-sen University (No. 12ykpy54), and the Outstanding Young Talents Project of Sun Yat-sen University Cancer Center (No. 04190101#).
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Additional information
Yue Lu acquired his M.D. and Ph.D. degree in Sapporo University Japan.
Rights and permissions
About this article
Cite this article
Wang, L., Xia, Zj., Zhang, Yj. et al. Radical surgery may be not an optimal treatment approach for pulmonary MALT lymphoma. Tumor Biol. 36, 6409–6416 (2015). https://doi.org/10.1007/s13277-015-3329-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-015-3329-y