Abstract
Background
Cardiovascular diseases are frequent in patients with obstructive sleep apnea (OSAS). There is evidence that the day–night pattern of myocardial infarction and sudden cardiac death observed in the general population is altered in patients with OSAS. This study investigates potential abnormalities in the circadian profiles of platelet activity in OSAS.
Methods
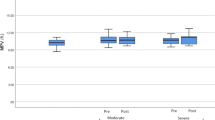
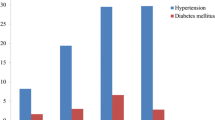
We studied 37 patients with OSAS [7 of whom were also studied after 3 months on continuous positive airway pressure (CPAP) treatment] and 11 controls. In each subject, we obtained six different blood samples during 24-h period (2200, 0200, 0600, 1000, 1400, and 1800 hours). Platelet activity was determined by flow cytometry immediately after sampling.
Results
We found that nocturnal platelet activity was significantly increased in patients with OSAS (p = 0.043) and that effective treatment with CPAP decreased platelet activity in these patients but differences just failed to reach statistical significance (p = 0.063).
Conclusions
OSAS is associated with increased platelet activity during the night, and that this appears to be improved by chronic use of CPAP. These results may contribute to explain the high prevalence of cardiovascular events during sleep in OSAS.


Similar content being viewed by others
References
Stradling JR, Davies RJ (2004) Sleep 1: obstructive sleep apnoea/hypopnoea syndrome: definitions, epidemiology, and natural history. Thorax 59:73–78
Sullivan CE, Berthon-Jones M, Issa FG, Eves L (1981) Reversal of obstructive sleep apnoea by continuous positive airway pressure applied through the nares. Lancet 1:862–865
Pack AI, Gislason T (2009) Obstructive sleep apnea and cardiovascular disease: a perspective and future directions. Prog Cardiovasc Dis 51:434–451
Marin JM, Carrizo SJ, Vicente E, Agusti AGN (2005) Long-term cardiovascular outcomes in men with obstructive sleep apnea. Effects of treatment with CPAP. Lancet 365 :1046–1053
Bradley TD, Floras JS (2009) Obstructive sleep apnoea and its cardiovascular consequences. Lancet 373:82–93
Somers VK, White DP, Amin R, Abraham WT, Costa F, Culebras A, Daniels S, Floras JS, Hunt CE, Olson LJ, Pickering TG, Russell R, Woo M, Young T (2008) Sleep apnea and cardiovascular disease: an American Heart Association/American College of Cardiology Foundation Scientific Statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council on Cardiovascular Nursing. In collaboration with the National Heart, Lung, and Blood Institute National Center on Sleep Disorders Research (National Institutes of Health). Circulation 118:1080–1111
Gozal D, Kheirandish-Gozal L (2008) Cardiovascular morbidity in obstructive sleep apnea: oxidative stress, inflammation, and much more. Am J Respir Crit Care Med 177:369–375
Somers VK, Dyken ME, Clary MP, Abboud FM (1995) Sympathetic neural mechanisms in obstructive sleep apnea. J Clin Invest 96:1904
Hedner J, Darpo B, Ejnell H, Carlson J, Caidahl K (1995) Reduction in sympathetic activity after long-term CPAP treatment in sleep apnoea: cardiovascular implications. Eur Respir J 8:222–229
Narkiewicz K, Kato M, Phillips BG, Pesek CA, Davison DE, Somers VK (1999) Nocturnal continuous positive airway pressure decreases daytime sympathetic traffic in obstructive sleep apnea. Circulation 100:2332–2335
Barcelo A, Miralles C, Barbe F, Vila M, Pons S, Agusti AGN (2000) Abnormal lipid peroxidation in patients with sleep apnea. Eur Respir J 16:644–647
Lavie L (2003) Obstructive sleep apnoea syndrome: an oxidative stress disorder. Sleep Med Rev 7:35–51
Ryan S, Taylor CT, McNicholas WT (2006) Predictors of elevated nuclear factor-kappaB-dependent genes in obstructive sleep apnea syndrome. Am J Respir Crit Care Med 174:824–830
von Känel R, Dimsdale JE (2003) Hemostatic alterations in patients with obstructive sleep apnea and the implications for cardiovascular disease. Chest 124:1956–1967
Muller JE, Stone PH, Turi ZG, Rutherford JD, Czeisler CA, Parker C, Poole WK, Passamani E, Roberts R, Robertson T (1985) Circadian variation in the frequency of onset of acute myocardial infarction. N Engl J Med 313:1315–1322
Goldberg RJ, Brady P, Muller JE, Chen ZY, de Groot M, Zonneveld P, Dalen JE (1990) Time of onset of symptoms of acute myocardial infarction. Am J Cardiol 66:140–144
Cohen MC, Rohtla KM, Lavery CE, Muller JE, Mittleman MA (1997) Meta-analysis of the morning excess of acute myocardial infarction and sudden cardiac death. Am J Cardiol 79:1512–1516
Huikuri HV, Niemela MJ, Ojala S, Rantala A, Ikaheimo MJ, Airaksinen KE (1994) Circadian rhythms of frequency domain measures of heart rate variability in healthy subjects and patients with coronary artery disease. Effects of arousal and upright posture. Circulation 90:121–126
Tofler GH, Brezinski D, Schafer AI, Czeisler CA, Rutherford JD, Willich SN, Gleason RE, Williams GH, Muller JE (1987) Concurrent morning increase in platelet aggregability and the risk of myocardial infarction and sudden cardiac death. N Engl J Med 316:1514–1518
Andreotti F, Davies GJ, Hackett DR, Khan MI, de Bart AC, Aber VR, Maseri A, Kluft C (1988) Major circadian fluctuations in fibrinolytic factors and possible relevance to time of onset of myocardial infarction, sudden cardiac death and stroke. Am J Cardiol 62:635–637
Muller JE (1999) Circadian variation in cardiovascular events. Am J Hypertens 12:35S–42S
Jovicic A, Mandic S (1991) Circadian variations of platelet aggregability and fibrinolytic activity in healthy subjects. Thromb Res 62:65–74
Jafri SM, VanRollins M, Ozawa T, Mammen EF, Goldberg AD, Goldstein S (1992) Circadian variation in platelet function in healthy volunteers. Am J Cardiol 69:951–954
Kuniyoshi FH, Garcia-Touchard A, Gami AS, Romero-Corral A, van der Walt C, Pusalavidyasagar S, Kara T, Caples SM, Pressman GS, Vasquez EC, Lopez-Jimenez F, Somers VK (2008) Day-night variation of acute myocardial infarction in obstructive sleep apnea. J Am Coll Cardiol 52:343–346
Gami AS, Howard DE, Olson EJ, Somers VK (2005) Day-night pattern of sudden death in obstructive sleep apnea. N Engl J Med 352:1206–1214
Schmitz G, Rothe G, Ruf A, Barlage S, Tschope D, Clemetson KJ, Goodall AH, Michelson AD, Nurden AT, Shankey TV (1998) European working group on clinical cell analysis: consensus protocol for the flow cytometric characterisation of platelet function. Thromb Haemost 79:885–896
Harrison P (2000) Progress in the assessment of platelet function. Br J Haematol 111:733–744
Burtis C, Ashwood E, Bruns D (2005) Tietz textbook of clinical chemistry and molecular diagnostics, 4th edn. Saunders Ed
Bode-Boger SM, Boger RH, Kielstein JT, Loffler M, Schaffer J, Frolich JC (2000) Role of endogenous nitric oxide in circadian blood pressure regulation in healthy humans and in patients with hypertension or atherosclerosis. J Investig Med 48:125–132
Pinotti M, Bertolucci C, Portaluppi F, Colognesi I, Frigato E, Foa A, Bernardi F (2005) Daily and circadian rhythms of tissue factor pathway inhibitor and factor VII activity. Arterioscler Thromb Vasc Biol 25:646–649
Undar L, Ertugrul C, Altunbas H, Akca S (1999) Circadian variations in natural coagulation inhibitors protein C, protein S and antithrombin in healthy men: a possible association with interleukin-6. Thromb Haemost 81:571–575
Madden LA, Vince RV, Sandstrom ME, Taylor L, McNaughton L, Laden G (2008) Microparticle-associated vascular adhesion molecule-1 and tissue factor follow a circadian rhythm in healthy human subjects. Thromb Haemost 99:909–915
Kapiotis S, Jilma B, Quehenberger P, Ruzicka K, Handler S, Speiser W (1997) Morning hypercoagulability and hypofibrinolysis. Diurnal variations in circulating activated factor VII, prothrombin fragment F1+2, and plasmin-plasmin inhibitor complex. Circulation 96:19–21
Otto ME, Svatikova A, Barretto RB, Santos S, Hoffmann M, Khandheria B, Somers V (2004) Early morning attenuation of endothelial function in healthy humans. Circulation 109:2507–2510
Keaney JF Jr, Weaver DR (2009) Vascular rhythms and adaptation: do your arteries know what time it is? Circulation 119:1463–1466
Decousus H, Boissier C, Perpoint B, Page Y, Mismetti P, Laporte S, Tardy B, Queneau P (1991) Circadian dynamics of coagulation and chronopathology of cardiovascular and cerebrovascular events. Future therapeutic implications for the treatment of these disorders? Ann NY Acad Sci 618:159–165
Maemura K, Takeda N, Nagai R (2007) Circadian rhythms in the CNS and peripheral clock disorders: role of the biological clock in cardiovascular diseases. J Pharmacol Sci 103:134–138
Walters J, Skene D, Hampton SM, Ferns GA (2003) Biological rhythms, endothelial health and cardiovascular disease. Med Sci Monit 9:RA1–RA8
Furlan R, Barbic F, Piazza S, Tinelli M, Seghizzi P, Malliani A (2000) Modifications of cardiac autonomic profile associated with a shift schedule of work. Circulation 102:1912–1916
Yamasaki F, Schwartz JE, Gerber LM, Warren K, Pickering TG (1998) Impact of shift work and race/ethnicity on the diurnal rhythm of blood pressure and catecholamines. Hypertension 32:417–423
Olson LJ, Olson EJ, Somers VK (2004) Obstructive sleep apnea and platelet activation: another potential link between sleep-disordered breathing and cardiovascular disease. Chest 126:339–341
Dean RT, Wilcox I (1993) Possible atherogenic effects of hypoxia during obstructive sleep apnea. Sleep 16:S15–S22
Rangemark C, Hedner JA, Carlson JA, Gleerup G, Winther K (1995) Platelet function and fibrinolytic activity in hypertensive and normotensive sleep apnea patients. Sleep 18:188–194
Hui DS, Ko FW, Fok JP, Chan MC, Li TS, Tomlinson B, Cheng G (2004) The effects of nasal continuous positive airway pressure on platelet activation in obstructive sleep apnea syndrome. Chest 125:1768–1775
Minoguchi K, Yokoe T, Tazaki T, Minoguchi H, Oda N, Tanaka A, Yamamoto M, Ohta S, O’Donnell CP, Adachi M (2007) Silent brain infarction and platelet activation in obstructive sleep apnea. Am J Respir Crit Care Med 175:612–617
Sanner BM, Konermann M, Tepel M, Groetz J, Mummenhoff C, Zidek W (2000) Platelet function in patients with obstructive sleep apnoea syndrome. Eur Respir J 16:648–652
Brezinski DA, Tofler GH, Muller JE, Pohjola-Sintonen S, Willich SN, Schafer AI, Czeisler CA, Williams GH (1988) Morning increase in platelet aggregability. Association with assumption of the upright posture. Circulation 78:35–40
Narkiewicz K, Somers VK (2003) Sympathetic nerve activity in obstructive sleep apnoea. Acta Physiol Scand 177:385–390
Acknowledgments
We thank Margalida Bosch and Mónica Iglesias for their assistance in the coordination of the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
The study is supported in part by SEPAR and Fondo de Investigaciones Sanitarias 07/906.
Rights and permissions
About this article
Cite this article
Barceló, A., Piérola, J., de la Peña, M. et al. Impaired circadian variation of platelet activity in patients with sleep apnea. Sleep Breath 16, 355–360 (2012). https://doi.org/10.1007/s11325-011-0501-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-011-0501-5