Abstract
Introduction
Subjects on methadone maintenance for drug addiction have been reported to have central sleep apnea (CSA). However, there are few reports of disordered breathing in patients receiving opioids for chronic pain.
Materials and methods
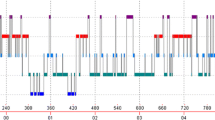
We report on six patients (ages 41–68, two females, body mass index 27–34, morphine equivalent doses 120–420 mg/day, Epworth Scales 7–21) referred to our sleep center receiving sustained release opioids for more than 6 months with excessive daytime sleepiness. CSA was defined as apnea–hypopnea index (AHI) more than 5 per hour with ≥50% central events. Bilevel (BLV) titration was done to determine settings and all patients were followed for at least 6 months on nocturnal BLV. AHI ranged 28.4–106 per hour. Time less than 90% O2 saturation ranged 1.8 min to 6.4 h. Four of the patients were treated with chronic BLV ventilation with settings ranging 12–16 cm H2O (inspiratory positive airway pressure)/4–8 cm H2O (expiratory positive airway pressure) with backup rate of 12–16. Among the four patients who used BLV treatment for at least 6 months, Epworth scores improved (by 4, 12, 5, and 9, respectively).
Conclusion
Treatment of opioid-associated CSA with BLV corrected nocturnal hypoxemia and reduced sleep fragmentation. Randomized controlled trials, with objective measures of daytime function, are recommended in opioid-induced CSA patients.


Similar content being viewed by others
References
Lanfranchi PA, Braghiroli A, Bosimini E (1999) Prognostic value of nocturnal Cheyne–Stokes respiration in chronic heart failure. Circulation 99:1435–1440
Bradley TD, Floras JS (2003) Sleep apnea and heart failure: part II: central sleep apnea. Circulation 107:1822–1826 doi:10.1161/01.CIR.0000061758.05044.64
Wang D, Teichtahl H, Drummer O (2005) Central sleep apnea in stable methadone maintenance treatment patients. Chest 128:1348–1356 doi:10.1378/chest.128.3.1348
Walker JM, Farney RJ, Rhondeau SM (2007) Chronic opioid use is a risk factor for the development of central sleep apnea and ataxic breathing. J Clin Sleep Med 3:455–461
Novak S, Nemeth WC, Lawson KA (2004) Trends in medical use and abuse of sustained-release opioid analgesics: a revisit. Pain Med 5:59–65 doi:10.1111/j.1526-4637.2004.04001.x
ARCOS US Department of Justice, Drug Enforcement Administration, Office of Diversion Control (2008) Retail drug summary. http://www.deadiversion.usdoj.gov/arcos/retail_drug_summary
Ballantyne JC, Mao J (2003) Opioid therapy for chronic pain. N Engl J Med 349:1943–1953 doi:10.1056/NEJMra025411
Sullivan CE, Issa FG, Berthon-Jones M et al (1981) Reversal of obstructive sleep apnea by continuous positive airway pressure applied through the nares. Lancet 1:862–865 doi:10.1016/S0140-6736(81)92140-1
Farney RJ, Walker JM, Cloward TV (2003) Sleep-disordered breathing associated with long-term opioid therapy. Chest 123:632–639 doi:10.1378/chest.123.2.632
Kryger MH, Roth R, Dement WC (2005) Principles and practice of sleep medicine. Elsevier Saunders, Philadelphia
Rechtshaffen A, Kales A (1968) A manual of standardized terminology: techniques and scoring system for sleep stages of human subjects. US Department of Health, Education and Welfare, Public Health Service-National Institutes of Health, Neurological Information Network, Bethesda
Santiago TV, Pugliese AC, Edelman NH (1977) Control of breathing during methadone addiction. Am J Med 62:347–354 doi:10.1016/0002-9343(77)90831-2
Teichtahl H, Wang D, Cunnington D (2005) Ventilatory responses to hypoxia and hypercapnia in stable methadone treatment patients. Chest 128:1339–1347 doi:10.1378/chest.128.3.1339
Bradly TD (2002) Crossing the threshold: implications for central sleep apnea. Am J Respir Crit Care Med 165:1203–1204 doi:10.1164/rccm.2203016
Skatrud JB, Dempsey JA (1983) Interaction of sleep state and chemical stimuli in sustaining rhythmic ventilation. J Appl Physiol 55:813–822
Santiago TV, Goldblatt K, Winters K (1980) Respiratory consequences of methadone: the response to added resistance to breathing. Am Rev Respir Dis 122:623–628
Cherniack NS (1981) Respiratory dysrhythmias during sleep. N Engl J Med 305:325–330
Berry RB, Gleeson K (1997) Respiratory arousal from sleep: mechanism and significance. Sleep 20:654–675
Sanders MH, Kern NB (1990) Obstructive sleep apnea treated by independently adjusted inspiratory and expiratory positive airway pressures via nasal mask. Chest 98:317–324 doi:10.1378/chest.98.2.317
Arzt M, Bradly D (2006) Treatment of sleep apnea in heart failure. Am J Respir Crit Care Med 173:1300–1308 doi:10.1164/rccm.200511-1745PP
Bradley TD, Logan AG, Kimoff RJ (2005) Continuous positive airway pressure for central sleep apnea and heart failure. N Engl J Med 353:2025–2033 doi:10.1056/NEJMoa051001
Naughton TM, Rahman A, Hara K et al (1995) Effect of continuous positive airway pressure on intrathoracic and left ventricular transmural pressures in patients with congestive heart failure. Circulation 91:1725–1731
Sin DD, Logan AG, Fitzgerald FS et al (2000) Effect of continuous positive airway pressure on cardiovascular outcomes in heart failure patients with and without Cheyne–Stokes respiration. Circulation 102:61–66
Goldberg A, Leger P, Hill N, Criner G (1999) Clinical indications for noninvasive positive pressure ventilation in chronic respiratory failure due to restrictive lung disease, COPD, and nocturnal hypoventilation: a consensus conference report. Chest 116:521–534 doi:10.1378/chest.116.2.521
Jones SE, Packham S, Hebden M (1998) Domiciliary nocturnal intermittent positive pressure ventilation in patients with respiratory failure due severe COPD: long-term follow-up and effect on survival. Thorax 53:495–498
Elliott MW, Simonds AK, Carroll MP (1992) Domiciliary nocturnal nasal intermittent positive pressure ventilation in hypercapnic respiratory failure due chronic obstructive pulmonary disease; effect on sleep and quality of life. Thorax 47:342–348
Krachman SL, Quaranta AJ, Berger TJ (1997) Effect of noninvasive positive pressure ventilation on gas exchange and sleep in COPD patients. Chest 112:623–628 doi:10.1378/chest.112.3.623
Krachman SL, Minai OA, Scharf SM (2008) Sleep abnormalities and treatment in emphysema. Proc Am Thorac Soc 5:536–542 doi:10.1513/pats.200708-134ET
Franklin KA, Eriksson P, Sahlin C (1997) Reversal of central sleep apnea with oxygen. Chest 111:163–169 doi:10.1378/chest.111.1.163
Acknowledgement
This paper was published in abstract form in the 22nd Annual Meeting of the Associated Professional Sleep Societies.
Conflict of interest
Authors have no conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Alattar, M.A., Scharf, S.M. Opioid-associated central sleep apnea: a case series. Sleep Breath 13, 201–206 (2009). https://doi.org/10.1007/s11325-008-0221-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-008-0221-7