Abstract
The time to first antibiotic dose (TFAD) has been mentioned as an important performance indicator in community-acquired pneumonia (CAP). However, the advice to minimise TFAD to 4 hours (4 h) is only based on database studies. We prospectively studied the effect of minimising the TFAD on the early clinical outcome of moderate–severe CAP. On admission, patients’ medical data and TFAD were recorded. Early clinical failure was expressed as the proportion of patients with clinical instability, admission to the intensive care unit (ICU) or mortality on day three. Of 166 patients included in the study, 27 patients (29.7%) with TFAD <4 h had early clinical failure compared to 23 patients (37.7%) with TFAD >4 h (odds ratio [OR] 0.69; 95% confidence interval [CI] 0.35–1.35). In multivariate analysis, the pneumonia severity index (OR 1.03; 95%CI 1.01–1.04), confusion (OR 2.63; 95%CI 1.14–6.06), Staphylococcus aureus infection (OR 7.26; 95%CI 1.33–39.69) and multilobar pneumonia (OR 2.40; 95%CI 1.11–5.22) but not TFAD were independently associated with early clinical failure. Clinical parameters on admission other than the TFAD predict early clinical outcome in moderate–severe CAP. In contrast to severe CAP necessitating treatment in the ICU directly, in the case of suspected moderate–severe CAP, there is time to establish a reliable diagnosis of CAP before antibiotics are administered. Therefore, the implementation of the TFAD as a performance indicator is not desirable.
Similar content being viewed by others
Introduction
Quality of care measurements and performance indicators are increasingly important in medical practice, in particular, in the treatment of high prevalence diseases [1]. Community-acquired pneumonia (CAP) is one of the leading causes of hospitalisation and mortality in the western world and is associated with high healthcare costs [2]. Therefore, performance indicators play an important role in the development of pneumonia care standards.
Current guidelines advise to minimise the time to first antibiotic dose (TFAD) in patients suspected of pneumonia. Moreover, the TFAD has frequently been mentioned as an important performance indicator in patients admitted because of pneumonia [3]. The European guidelines’ recommendation is to initiate antibiotics within the first two hours of hospitalisation, whereas the current Infectious Disease Society of America/American Thoracic Society consensus guidelines advise the first antibiotic dose to be administered while the patient is still in the emergency department [4, 5]. These recommendations are mainly based on two retrospective database studies demonstrating an association between antibiotic timing and severity-adjusted outcome in pneumonia [6, 7]. Therefore, as the advice to minimise the TFAD is only based on grade C level of evidence and more recent studies do not support their findings, the validity of these studies has been questioned [4, 8–12]. Additionally, minimising the TFAD is associated with drawbacks as well. Adopting the TFAD as a performance indicator may lead to the prioritisation of pneumonia patients over others and unnecessary antibiotic treatment for patients who ultimately receive another diagnosis (e.g. congestive heart failure), contributing to an increase in antibiotic use, side-effects, resistance and costs. Another concern is that patients may receive inappropriate antibiotics for suspected pneumonia due to time pressure [13, 14]. This is illustrated by a recent study which shows that linking TFAD within four hours (4 h) to financial compensation may result in less optimal care [15].
Preferably, performance indicators are based on recommendations with adequate scientific proof of their effectiveness, safety and efficiency [16]. The need for evidence is even more urgent in view of today’s trend to use performance indicators as the basis for public reporting and plans to implement quality measures such as the TFAD in pay-for-performance programmes [17]. When adopting the TFAD as a quality measure in pay-for-performance programmes for the treatment of CAP, more studies on the impact of the TFAD on outcome are needed. Therefore, we prospectively studied the effect of the TFAD on early clinical outcome in patients hospitalised with moderate–severe CAP admitted to general medical and pulmonary wards.
Methods
Patients and setting
The prospective cohort of patients in this study was derived from a multicentre prospective randomised controlled trial on the cost-effectiveness of an early switch from parenteral to oral therapy for severe CAP [18]. Patients were included during a three-year period from July 2000 to June 2003 in University Medical Centres and their affiliated teaching hospitals in the Netherlands. All adult patients (age 18 years and above) admitted to the hospital because of CAP were eligible for inclusion. CAP was defined as at least two symptoms of acute lower respiratory tract infection with onset before admission and a new or progressive pulmonary infiltrate on a chest radiograph. Written and oral informed consent was retrieved from all of the patients included. Moderate–severe pneumonia was defined as a pneumonia severity index score >90 and necessitating admission to the general medical or pulmonary ward, without immediate treatment in the intensive care unit (ICU) [19, 20]. Antibiotic treatment was based on the Dutch guidelines for pneumonia management [21].
Data collection and definitions
For the current study, patients were included at the time of hospital admission and were followed for at least three days after diagnosis. On admission, data were collected on demographics, comorbidity, antibiotic use prior to admission, duration of symptoms before admission, pneumonia severity scores, the TFAD, site of administration of first antibiotic dose and initial choice of antibiotics [20, 22]. In addition, cultures, serology and urinary antigen tests were performed to establish an aetiological diagnosis. During follow-up, in-hospital clinical data were recorded. On the third day of admission, patients were evaluated for clinical outcome by means of clinical failure, including clinical instability, mortality and admission to the ICU. Clinical instability was defined as: respiratory rate >25/min, peripheral oxygen saturation <90%, partial pressure of arterial oxygen <60 mmHg, haemodynamic instability or altered mental status [23]. Indication for ICU admission was the need for mechanical ventilation or vasopressors, as determined by the treating physician [4, 5].
Microbiological evaluation
Details of the microbiological procedures have been described earlier [18]. In short, sputum and blood samples were collected, cultured and evaluated according to standard procedures. Urinary antigen tests (Binax Inc., Portland, ME) were used to detect antigens of Legionella pneumophila and Streptococcus pneumoniae. Acute and convalescent sera were collected and tested for Mycoplasma pneumoniae, L. pneumophila and Chlamydia pneumoniae. Pathogenic micro-organisms cultured from blood or sputum detected by urinary antigen test or a seroconversion were considered to be the cause of the episode of pneumonia.
Definitions of antibiotic treatment
The TFAD is defined as the time elapsed between presentation to the emergency department and first antibiotic administration, as recorded on the drug accountability lists kept by the nursing staff. The ward to needle time was defined as the time elapsed between admission to the ward and the first antibiotic administration. Appropriate empiric antibiotic treatment was defined as all identified pathogens being susceptible for the antibiotics administered. In case no aetiology was determined, empiric antibiotic treatment was also considered as appropriate.
Analytical approach
Patients with antibiotic treatment prior to hospital admission were excluded from the analysis. To explore potential confounders, the baseline characteristics of patients who received antibiotics within four hours (<4 h) after admission to the hospital were compared to those of patients with the first antibiotic dose after four hours of admission (>4 h). A variation of >10% in baseline characteristics was estimated to be relevant. The objective of the study was to evaluate the influence of the TFAD on early clinical outcome. Early clinical failure was defined as clinical instability, admission to the ICU or mortality on day three of hospitalisation. Patients with TFAD <4 h were compared to patients with TFAD >4 h for differences in the rate of early clinical failure. In addition, the time–effect relation in the TFAD and early clinical failure was explored. Finally, multivariable assessment of clinical parameters on admission predictive of clinical failure on day three of admission was performed [23].
Statistical methods
For comparisons between subgroups of patients with continuous scaled data, we used Student’s t-test and for skewed scaled data, the Mann-Whitney U-test was used. Categorical variables were compared using the chi-square test and by estimation of the odds ratio (OR) with corresponding 95% confidence intervals (CI) for the selected patients. The ideal TFAD was assessed by using stepwise cut-off point’s at 1-h intervals up to 8 h after admission. Spearman’s correlation was used to estimate a time–effect relationship between the TFAD and clinical failure. Multivariate logistic regression modelling was used and significant interactions were included in the model with a P-value <0.10 as the threshold. Forward selection was performed to verify whether any previously deleted potentially relevant characteristic had been eliminated incorrectly from the model. All analytical procedures were performed using SPSS v15.0 for Windows (SPSS Inc., Chicago, IL).
Results
Baseline characteristics of the study population
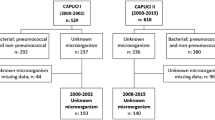
Of 200 patients admitted with moderate–severe CAP to one of the participating hospitals, the TFAD could be assessed appropriately. Thirty-four (17%) patients had received antibiotic treatment prior to hospitalisation and were consequently excluded for further analysis, leaving 166 patients for analysis. In 152 (91.6%) patients, follow-up until the third day of admission was accomplished (Fig. 1). Ninety-five (57.2%) patients presented to the emergency department of the University Medical Center Utrecht, the Netherlands, and 71 (42.8%) to one of its affiliated regional teaching hospitals. Patients admitted to one of the teaching hospitals received more often their first antibiotic dose in the emergency room and slightly more severely ill patients were admitted to the University Medical Center; however, this was not statistically significant. The mean pneumonia severity index score in the study population was 108.8 (±24.1 standard deviation [SD]) and the mean age was 67.2 years (±14.5 SD). One hundred and seven (64.5%) patients had at least one co-morbid illness, such as congestive heart failure, neoplasm, cerebrovascular disease, chronic renal failure or chronic obstructive pulmonary disease. The aetiology could be determined in 79 (47.6%) patients. S. pneumoniae was the most frequently identified pathogen (38 [22.9%] patients). Beta-lactam monotherapy was the most frequently instituted initial antibiotic therapy in 131 (79.4%) patients and 30 (18.2%) patients received combination therapy with beta-lactam and macrolide antibiotics. In 152 (91.6%) patients, empiric antibiotic treatment was appropriate, of which 91 (59.9%) patients received appropriate antibiotics within 4 h (Table 1).
TFAD and the ‘4 hour rule’
Overall, the median TFAD was 3 h 12 min. In 100 patients (60.2%), the TFAD was <4 h (median 2 h 23 min; range 0 h 25 min to 3 h 46 min) and in 66 (39.8%) patients it was >4 h (median 5 h 17 min; range 4 h 00 min to 73 h 15 min). The ward to needle time was 0 h 30 min (±0 h 52 min SD) in patients with first antibiotic dose <4 h and 1 h 27 min (±8 h 19 min SD) in patients with delayed antibiotic administration (P < 0.01). No important differences in patients’ characteristics, pneumonia severity scores, clinical signs, symptoms or causative pathogens were observed between both groups (Table 1). Importantly, no relevant difference in the duration of symptoms before hospital admission or appropriateness of the initiated antibiotics in patients with or without TFAD <4 h could be identified. However, a baseline difference in the prevalence of cerebrovascular disease and chronic obstructive pulmonary disease was identified (Table 1). Patients with chronic obstructive pulmonary disease as a co-morbid illness had significantly more often early antibiotic administration (43.0% versus 27.3%), whereas patients with cerebrovascular disease had more often delayed administration of first antibiotic dose (13.6% versus 3.0%).
The effect of the TFAD on early clinical outcome
Of the 152 patients followed until day three of hospitalisation, the TFAD was <4 h in 91 (59.9%) patients and >4 h in 61 (40.1%) patients. Twenty-four patients (26.4%) with early antibiotic administration had clinical instability on day three, as compared to 22 (36.1%) patients with TFAD >4 h. This was not statistically significant (OR 0.65; 95% CI 0.32–1.31; P = 0.22). There was also no significant difference in the rates of early clinical failure for patients with TFAD <4 h and patients with TFAD >4 h (OR 0.69; 95% CI 0.35–1.35; P = 0.28) (Table 2). Figure 2 shows the influence of minimising the TFAD on early clinical outcome evaluated by stepwisely increasing the TFAD with 1-h intervals up to 8 h after admission. Rates for early clinical failure did not increase substantially by increasing the TFAD stepwisely up to 8 h. Furthermore, no time–effect relation was observed between the TFAD and early clinical failure (Spearman’s correlation 0.12, P = 0.13) (Fig. 2).
Factors predictive of early clinical failure
In the univariate and multivariate analysis, we explored parameters on admission predictive for early clinical failure in severe CAP. The TFAD was not independently associated with early clinical failure. However, the pneumonia severity index score on admission (OR 1.03; 95% CI 1.01–1.04), confusion on admission (OR 2.63; 95% CI 1.14–6.06), S. aureus infection (OR 7.26; 95% CI 1.33–39.69) and multilobar pneumonia (OR 2.40; 95% CI 1.11–5.22) were independently predictive for a less favourable clinical outcome on day three of hospitalisation (P ≤ 0.03) (Table 3). As mentioned before, patients with chronic obstructive pulmonary disease as a co-morbidity had more often earlier antibiotic administrated, while patients with cerebrovascular disease had more often delayed antibiotic administration (Table 1). Nevertheless, co-morbidity as chronic obstructive pulmonary disease and cerebrovascular disease are not independently associated with early clinical failure and, therefore, are ruled out as potential confounders (Table 3).
Discussion
We demonstrated that TFAD within four hours was not predictive for early clinical failure in moderate–severe CAP. Additionally, the effect of postponing the administration of antibiotics up to 8 h after admission was not associated with an effect on the early clinical outcome. Furthermore, no time–effect relation was observed between the TFAD and early clinical failure.
Therefore, this report suggests that earlier antibiotic administration has no demonstrable beneficial effect on the early achievement of clinical stability or cure in patients admitted with moderate–severe CAP admitted to general medical or pulmonary wards.
Our study differs from previous studies in several important aspects. The strengths of this study were the prospective data collection in a multicentre setting and the strict patient selection; only patients with moderate-severe CAP primarily treated in general wards were included. Two large retrospective database studies reported the TFAD as an important predictor for mortality in patients with CAP. Meehan et al. demonstrated that antibiotic delivery time less than 8 h was associated with a 15% lower odds of 30-day mortality (95% CI 075–0.96) [6]. In addition, Houck et al. described that antibiotic treatment within 4 h was associated with decreased mortality and length of hospital stay [7]. These results have led to the implementation of minimising the TFAD as a recommendation in guidelines on CAP. Yet, the major weakness of these studies was the retrospective study design. Moreover, correction for pre-hospital parameters such as antibiotic use and duration of symptoms before hospital admission was not performed, so heterogeneity in the study population could have led to a confounding effect [10]. Likewise, Battleman et al. examined the TFAD in patients hospitalised with pneumonia and concluded that timely antibiotic administration was associated with a shorter length of hospital stay [24], while several other studies could not identify early antibiotic administration as an independent predictor for diminished mortality [9, 10, 12, 15, 25–27].
The influence of timely antibiotic administration on early clinical failure has been studied twice before [10, 11]. The findings of these reports are in agreement with our results: the TFAD does not influence the rate of clinical failure. In contrast to our study, these studies included patients with mild CAP as well. However, in a heterogeneous study population of patients with mild to severe pneumonia, the effect of minimising the TFAD on clinical stability may be underestimated, since patients with more severe pneumonia often receive priority in treatment in the emergency room [6, 10]. For purpose of the current study, we excluded patients with severe CAP directly admitted to the ICU, minimising the potential confounding effect of early antibiotic administration in the most critically ill patients. Moreover, the debate on minimising the TFAD with associated drawbacks is particularly applicable to large groups of patients admitted with moderate–severe CAP to general wards instead of the few admitted to the ICU directly.
In addition, the timing of antibiotic administration is influenced by the difficulty of diagnosis. In line with other studies, patients in our cohort with cerebrovascular disease often receive their antibiotics later, whereas patients with chronic obstructive pulmonary disease receive antibiotics earlier [12]. This can be partly explained by the difficulty in diagnosing a respiratory tract infection in the first patient group.
These issues raised illustrate the complexity in studying the predictive value of the TFAD on outcome in patients hospitalised with CAP. Efforts to promote the early administration of appropriate antibiotics in patients hospitalised with CAP make good clinical sense. However, our results and previous studies emphasise the difficulty in demonstrating the attributable impact of these procedures on clinical outcome. It may be inappropriate to expect hospitals to deliver antibiotics to all patients suspected of pneumonia within four hours of presentation. This approach would lead to the administration of antibiotics to many patients in whom the diagnosis of pneumonia is still in doubt, leading to an increasing rate of inappropriate antibiotic use, antibiotic resistance, antibiotic-related side-effects and an decrease in the yield of subsequently required diagnostic tests [28]. Furthermore, although some patients may benefit of the early administration of antibiotics, there is a risk to other patients who are treated concurrently and may not receive the same priority as patients with suspected pneumonia [13, 14].
Some limitations of the current study must be acknowledged. Certainly, the study population is much smaller than the population included in the large database studies, although the accuracy of diagnosis in this prospective study is very high as compared to the coding database studies. As a valid diagnosis of CAP is crucial for studies on this topic, it is probably better to rely on the results of several smaller prospective studies together than on a single large database study. Owing to the fact that the current study was part of a therapeutic trial in severe CAP with an intervention on the third day, results on long-term outcome would probably not be reliable and are, therefore, not presented. We are aware that the absence of early deterioration does not necessarily imply a favourable long-term outcome. However, early clinical outcome is an appropriate outcome measure for evaluating therapeutic strategies initiated on admission [29]. Obviously, a randomised controlled trial is the ideal study design to investigate the impact of minimising the TFAD. However, intentionally delaying antibiotic therapy in pneumonia would be unethical.
Nevertheless, there must be a basis of recommendations with adequate scientific proof of their evidence, safety and feasibility to develop performance indicators [16], particularly because the introduction of performance indicators may have a large impact on clinical practice. Studies reported that antibiotic administration within four hours in the emergency department was often not feasible due to crowding [30]. In our opinion, at this moment, there seems not to be sufficient evidence in the published literature to justify the implementation of the TFAD as a performance indicator and penalise hospitals for not being in compliance with current guidelines on this behalf. To improve care in the treatment of pneumonia, it is probably better to focus on interventions based on established evidence, such as the correction of hypotension in septic shock or timely oxygen administration [31, 32]. These interventions seem to be better targets for performance indicators than minimising the TFAD. Furthermore, since CAP can be difficult to diagnose due to the wide variety of clinical symptoms and differential diagnoses, future research needs to focus on the development and implementation of adequate diagnostic algorithms to rapidly discriminate CAP from other clinical syndromes. A more rapid and reliable diagnosis of CAP may lead to antibiotics administration early in the course of disease without increasing unnecessary antibiotic use as enhanced by the implementation of minimising the TFAD as a performance indicator.
In conclusion, clinical parameters on admission other than the TFAD predict early clinical outcome in patients with moderate–severe CAP admitted to general wards. In contrast to severe CAP necessitating treatment in the ICU directly, in the case of suspected moderate–severe CAP, one can take time to establish a reliable diagnosis before the administration of antibiotics. Therefore, implementation of the TFAD as a performance indicator may not be desirable.
References
Mainz J (2003) Developing evidence-based clinical indicators: a state of the art methods primer. Int J Qual Health Care 15(Suppl 1):i5–i11. doi:10.1093/intqhc/mzg084
Fry AM, Shay DK, Holman RC et al (2005) Trends in hospitalizations for pneumonia among persons aged 65 years or older in the United States, 1988–2002. JAMA 294:2712–2719. doi:10.1001/jama.294.21.2712
Pines JM (2006) Profiles in patient safety: antibiotic timing in pneumonia and pay-for-performance. Acad Emerg Med 13:787–790
Mandell LA, Wunderink RG, Anzueto A et al (2007) Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis 44(Suppl 2):S27–S72. doi:10.1086/511159
Woodhead M, Blasi F, Ewig S et al (2005) Guidelines for the management of adult lower respiratory tract infections. Eur Respir J 26:1138–1180. doi:10.1183/09031936.05.00055705
Meehan TP, Fine MJ, Krumholz HM et al (1997) Quality of care, process, and outcomes in elderly patients with pneumonia. JAMA 278(23):2080–2084. doi:10.1001/jama.278.23.2080
Houck PM, Bratzler DW, Nsa W et al (2004) Timing of antibiotic administration and outcomes for Medicare patients hospitalized with community-acquired pneumonia. Arch Intern Med 164:637–644. doi:10.1001/archinte.164.6.637
Marrie TJ, Wu L (2005) Factors influencing in-hospital mortality in community-acquired pneumonia: a prospective study of patients not initially admitted to the ICU. Chest 127:1260–1270. doi:10.1378/chest.127.4.1260
Benenson R, Magalski A, Cavanaugh S et al (1999) Effects of a pneumonia clinical pathway on time to antibiotic treatment, length of stay, and mortality. Acad Emerg Med 6:1243–1248. doi:10.1111/j.1553-2712.1999.tb00140.x
Silber SH, Garrett C, Singh R et al (2003) Early administration of antibiotics does not shorten time to clinical stability in patients with moderate-to-severe community-acquired pneumonia. Chest 124:1798–1804. doi:10.1378/chest.124.5.1798
Dedier J, Singer DE, Chang Y et al (2001) Processes of care, illness severity, and outcomes in the management of community-acquired pneumonia at academic hospitals. Arch Intern Med 161:2099–2104. doi:10.1001/archinte.161.17.2099
Waterer GW, Kessler LA, Wunderink RG (2006) Delayed administration of antibiotics and atypical presentation in community-acquired pneumonia. Chest 130:11–15. doi:10.1378/chest.130.1.11
Pines JM, Hollander JE, Datner EM et al (2006) Pay for performance for antibiotic timing in pneumonia: caveat emptor. Jt Comm J Qual Patient Saf 32:531–535
Mitka M (2007) JCAHO tweaks emergency departments’ pneumonia treatment standards. JAMA 297:1758–1759. doi:10.1001/jama.297.16.1758
Kanwar M, Brar N, Khatib R et al (2007) Misdiagnosis of community-acquired pneumonia and inappropriate utilization of antibiotics: side effects of the 4-h antibiotic administration rule. Chest 131:1865–1869. doi:10.1378/chest.07-0164
Wollersheim H, Hermens R, Hulscher M et al (2007) Clinical indicators: development and applications. Neth J Med 65:15–22
Lindenauer PK, Remus D, Roman S et al (2007) Public reporting and pay for performance in hospital quality improvement. N Engl J Med 356:486–496. doi:10.1056/NEJMsa064964
Oosterheert JJ, Bonten MJ, Schneider MM et al (2006) Effectiveness of early switch from intravenous to oral antibiotics in severe community acquired pneumonia: multicentre randomised trial. BMJ 333:1193. doi:10.1136/bmj.38993.560984.BE
Niederman MS, Mandell LA, Anzueto A et al (2001) Guidelines for the management of adults with community-acquired pneumonia. Diagnosis, assessment of severity, antimicrobial therapy, and prevention. Am J Respir Crit Care Med 163:1730–1754
Fine MJ, Auble TE, Yealy DM et al (1997) A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med 336:243–250. doi:10.1056/NEJM199701233360402
Schouten JA, Prins JM, Bonten MJ et al (2005) Revised SWAB guidelines for antimicrobial therapy of community-acquired pneumonia. Neth J Med 63:323–335
Lim WS, van der Eerden MM, Laing R et al (2003) Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax 58:377–382. doi:10.1136/thorax.58.5.377
Halm EA, Fine MJ, Marrie TJ et al (1998) Time to clinical stability in patients hospitalized with community-acquired pneumonia: implications for practice guidelines. JAMA 279:1452–1457. doi:10.1001/jama.279.18.1452
Battleman DS, Callahan M, Thaler HT (2002) Rapid antibiotic delivery and appropriate antibiotic selection reduce length of hospital stay of patients with community-acquired pneumonia: link between quality of care and resource utilization. Arch Intern Med 162:682–688. doi:10.1001/archinte.162.6.682
Barlow G, Nathwani D, Williams F et al (2007) Reducing door-to-antibiotic time in community-acquired pneumonia: controlled before-and-after evaluation and cost-effectiveness analysis. Thorax 62:67–74. doi:10.1136/thx.2005.056689
Schaaf B, Kruse J, Rupp J et al (2007) Sepsis severity predicts outcome in community-acquired pneumococcal pneumonia. Eur Respir J 30:517–524. doi:10.1183/09031936.00021007
Ziss DR, Stowers A, Feild C (2003) Community-acquired pneumonia: compliance with centers for Medicare and Medicaid services, national guidelines, and factors associated with outcome. South Med J 96:949–959. doi:10.1097/01.SMJ.0000051147.88941.FB
Metersky ML, Sweeney TA, Getzow MB et al (2006) Antibiotic timing and diagnostic uncertainty in Medicare patients with pneumonia: is it reasonable to expect all patients to receive antibiotics within 4 hours? Chest 130:16–21. doi:10.1378/chest.130.1.16
Mortensen EM, Coley CM, Singer DE et al (2002) Causes of death for patients with community-acquired pneumonia: results from the Pneumonia Patient Outcomes Research Team cohort study. Arch Intern Med 162:1059–1064. doi:10.1001/archinte.162.9.1059
Fee C, Weber EJ (2007) Identification of 90% of patients ultimately diagnosed with community-acquired pneumonia within four hours of emergency department arrival may not be feasible. Ann Emerg Med 49:553–559. doi:10.1016/j.annemergmed.2006.11.008
Blot SI, Rodriguez A, Solé-Violán J et al (2007) Effects of delayed oxygenation assessment on time to antibiotic delivery and mortality in patients with severe community-acquired pneumonia. Crit Care Med 35:2509–2514. doi:10.1097/01.CCM.0000266825.19629.BA
Kumar A, Haery C, Paladugu B et al (2006) The duration of hypotension before the initiation of antibiotic treatment is a critical determinant of survival in a murine model of Escherichia coli septic shock: association with serum lactate and inflammatory cytokine levels. J Infect Dis 193:251–258. doi:10.1086/498909
Acknowledgement
We thank all of the patients and investigators who participated in this trial.
Transparency declarations
The study was approved by the medical ethics committees of all of the participating hospitals.
Conflict of interest statement
All authors: no conflicts.
Financial support
All authors: no financial support.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Bruns, A.H.W., Oosterheert, J.J., Hustinx, W.N.M. et al. Time for first antibiotic dose is not predictive for the early clinical failure of moderate–severe community-acquired pneumonia. Eur J Clin Microbiol Infect Dis 28, 913–919 (2009). https://doi.org/10.1007/s10096-009-0724-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-009-0724-6