Abstract
Background
Fibrosing interstitial pneumonias (IPs) include idiopathic pulmonary fibrosis (IPF) and nonspecific interstitial pneumonia (NSIP). It has been suggested that oxidative damage plays a role in the pathophysiology of idiopathic interstitial pneumonias. Diffuse alveolar hemorrhage (DAH) can cause oxidative stress. Accordingly, we hypothesized that episodes of DAH might trigger fibrosing IP development.
Methods
Patients using coumarins with confirmed DAH were retrospectively gathered during a 9 year period and reviewed for the development of IPF or fibrosing NSIP.
Results
A total of 65 patients with DAH could finally be included, 31 (48 %) of whom subsequently developed a fibrosing IP. The majority of these 31 patients developed the fibrosing IP within 3 years after DAH confirmation. A total of 41 (63 %) patients died within 3.0 ± 0.9 (range 1.3–4.7) years after the DAH diagnosis had been confirmed. Twenty-two of the deceased (54 %) had finally developed fibrosing IP.
Conclusions
Almost half of the patients with established episodes of DAH developed fibrosing IP; therefore it seems that DAH might be a trigger for the development of fibrosing IP. This observation warrants prospective studies to further evaluate the clinical impact of these findings.
Similar content being viewed by others
Introduction
Idiopathic interstitial pneumonias (IIPs) are considered to be multifaceted diseases with a strong interaction between genetic makeup and environmental factors. The most frequently occurring interstitial pneumonias (IPs) are idiopathic pulmonary fibrosis (IPF) and nonspecific interstitial pneumonia (NSIP). They are characterized by abnormal repair and airway remodeling and associated with increased proinflammatory and profibrotic signals. Some patients with a disease in the IIP spectrum are difficult to classify, often due to mixed patterns of lung injury [1, 2]. The clinical picture and prognosis are variable. Some patients remain stable or improve with treatment, but the majority evolves to end-stage fibrosis and eventually dies from the disease.
The process of arriving at a multidisciplinary diagnosis in a patient with IIP is dynamic, requiring close communication between clinician, radiologist, and pathologist [1, 3, 4]. IIPs may have an acute or subacute presentation, or an acute exacerbation may occur in a previously subclinical or unrecognized chronic IIP [5, 6].
It has been suggested that oxidative damage plays a role in the pathophysiology of various diseases, including IIPs [7, 8]. Oxidative stress and inflammation can be caused by accumulation of iron in the lungs and is associated with episodes of diffuse alveolar hemorrhage (DAH). DAH refers to a clinical syndrome presenting with hemoptysis, anemia, and progressive hypoxemia, resulting in red blood cell accumulation in the distal air spaces. A number of conditions are associated with this clinical syndrome, including vasculitis, diffuse alveolar damage (DAD), and drug-induced DAH [7]. It is important to prevent or recognize DAH at an early stage to avoid irreversible damage. The presence of DAH should be considered particularly in critically ill patients with unexplained lung opacities.
Drug-induced DAH events may occur as a result of over-anticoagulation due to coumarin sensitivity, resulting in a relative vitamin K deficiency. Coumarin-based oral anticoagulants, acting as vitamin K antagonists, have been the most commonly prescribed drugs for therapy and prophylaxis of thromboembolic conditions, such as venous thrombosis, pulmonary embolism, chronic atrial fibrillation, prosthetic heart valves, and other cardiovascular conditions [9]. Recently, we found that in patients using oral anticoagulation therapy, DAH was associated with the presence of vitamin K epoxide reductase complex 1 (VKORC1) and cytochrome P450 (CYP) 2C9 variant alleles [9]. It also can occur as a result of the ingestion or inhalation of so-called super-warfarin, (illicit) drugs, or toxic fumes [10–13].
In our clinic, we have noticed that a substantial number of patients with fibrosing IP used oral anticoagulants, mainly because of a cardiac event in the past. As a consequence, several of them suffered from episodes of DAH. Hence, the question was raised whether these episodes of DAH might trigger the development of fibrosing IP. The purpose of this retrospective follow-up study was to identify cases with established DAH who developed fibrosing IP.
Patients and Methods
We retrospectively reviewed the medical records of patients with one or more established episode(s) of DAH who used coumarin (n = 71) and were seen at the Maastricht University Medical Centre (Maastricht, the Netherlands) from 2002 through 2011, to assess whether they developed fibrosing IP. Patients with pre-existent pulmonary diseases, such as sarcoidosis (n = 3), Wegener’s disease (n = 2), and COPD (n = 1) were excluded. The majority of the finally included 65 patients (89 %; n = 58) underwent treatment for cardiovascular problems. The indications for coumarin use ranged from atrial flutter or fibrillation (n = 23) to myocardial infarction (n = 13), chronic heart failure or cardiomyopathy (n = 14), pulmonary embolism (n = 5), valve replacement surgery (n = 8), deep-vein thrombosis (n = 1), and hip replacement (n = 1). The diagnosis of DAH had been established on the bases of bronchoalveolar lavage fluid (BALF), as previously reported [9]. More than 20 % of iron-stain-positive macrophages were considered to be indicative of alveolar hemorrhage [14, 15].
The diagnosis of fibrosing IP had been established from high-resolution computed tomography (HRCT) specimens by an experienced radiologist (JAV) according to the international guidelines [1, 3, 16]. Various pathologic patterns in biopsies, e.g., usual interstitial pneumonia (UIP) or NSIP or both were considered to indicate fibrosing IP [1, 3].
The study protocol was approved by the Medical Ethics Board of the Maastricht University Medical Centre (MEC azM/UM B04.1.1168).
Imaging and Diagnosis
HRCT data and/or autopsy results were retrospectively collected and evaluated for the presence of pulmonary fibrosis as specified in the international consensus statement on pulmonary fibrosis [3]. On HRCT, lung fibrosis was suggested when lung architecture distortion was seen together with irregular reticular opacities, possibly associated with traction bronchiectasis/bronchiolectasis and honeycombing. When these HRCT features were seen in the subpleural and basal part of both lungs, they were considered to indicate a UIP pattern when honeycombing with or without traction bronchiectasis was present, or as a possible UIP pattern when these were not present [3].
When available, older CT scans were evaluated for the presence of DAH. DAH was considered if multiple confluent areas of ground-glass opacity and lung consolidation were present, especially when more pronounced in the dependent lung areas.
Lung Function Tests
Forced vital capacity (FVC) was measured with a pneumotachograph (Masterlab, Jaeger, Würzburg, Germany). The diffusing capacity for carbon monoxide (DLCO) was measured by the single-breath method (Masterlab). Values were expressed as a percentage of predicted values. The cutoff value for the DLCO and FVC was <80 % of predicted (≥80 % was normal) [17].
Statistical Analysis
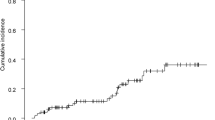
Statistical analyses were performed with SPSS 15.0 (SPSS. Inc., Chicago, IL) for Windows. Kaplan-Meier was used to calculate survival estimates.
Results
Available follow-up HRCT scans (n = 47) of the DAH patients were retrospectively reviewed. The diagnosis of fibrosing IP was based on established HRCT criteria (n = 29) and confirmed by lung biopsy or autopsy in five patients, whereas for three patients only lung biopsy specimens were available (Table 1) [2]. Of the 31 patients with fibrosing IP, 20 displayed a UIP pattern.
The characteristics are summarized in Table 1. Only nine patients showed signs of infection in the BALF (intracellular bacteria >2 %; six patients with fibrosing IP and three without fibrosing IP) [18].
Lung function tests had been performed in only in three cases of the group without fibrosing IP. In the group with fibrosing IP, the mean DLCO (percentage of predicted value) was 52.9 (13.9) and FVC (percentage of predicted value) was 91.1 (17.4). Note that the patients were tested in a stable period of the disease and not during a DAH episode.
Of the 65 included patients with at least one established episode of DAH, 31 (48 %) subsequently developed fibrosing IP. The 1 year frequency of fibrosing IP in the group of patients with DAH was 48 % (n = 15), whereas the 3 year frequency was 65 % (n = 20), and that for 4 years and longer 35 % (n = 11). A total of 41 (63 %) patients died within 3.0 ± 0.9 (range 1.3–4.7) years after the DAH episode had been established, and 3.0 ± 1.5 (range 0.1–5.9) years after fibrosing IP had been detected. Twenty-two of the deceased patients (54 %) had developed fibrosing IP.
In seven of the cases, we studied the time between the established episode of DAH and death was less than 6 months. This was due to comorbidities, such as malignancies in two patients, or the severity of the initial condition, for instance myocardial infarction and/or cardiomyopathy. No follow-up HRCT and/or lung biopsy was available for 12 of the included patients, and four patients classified as not having developed fibrosing IPs, were lost to follow-up.
Drug-use of the selected patients was reviewed, especially drugs associated with drug-induced pneumonitis. There were five patients who used amiodarone, three of whom developed fibrosing IP, so this cannot be excluded as a cofactor in the development of fibrosing IP in these patients. Nine of the DAH patients received vitamin K supplementation, two of whom (22 %) had died to date. One of these deceased patients had developed fibrosing IP, and both had an initial cardiological condition (cardiomyopathy and valve replacement surgery, respectively).
Discussion
To the best of our knowledge, this was the first study to evaluate the progress to fibrosing IP in a population of patients with DAH. The incidence of fibrosing IP in our DAH population was high compared with the incidence reported for a general population (48 vs. ~0.02 %, respectively) [19–23]. The actual incidence of the development of fibrosing IP in the patients included in our study could even be higher, as the time between the established episode of DAH and death was rather short in seven cases, and follow-up data was unavailable for 16 of the studied cases. Acute deterioration of fibrosing IP may occur without an identifiable cause, but often in combination with coronary problems (e.g., heart failure, myocardial infarction), pulmonary embolisms, or infections [24, 25].
The majority of the studied patients (n = 58, 89 %) suffered from various cardiovascular or underlying cardiovascular problems, which also was the main reason to initiate oral anticoagulants or coumarin (Table 1). After the DAH episode, 48 % of the patients subsequently developed fibrosing IP. It is tempting to speculate that the DAH episodes could at least be one of the triggers of the development of fibrosing IP or that they made any possible pre-existing subclinical fibrosis progress more rapidly. This suggests a possible association between DAH and subsequent fibrosing IP, and one might obviously expect that the number of DAH episodes could influence the development of fibrosing IP as well. However, in the present retrospective study we were not fully informed about the exact number of DAH episodes, because we cannot exclude that some of the patients went through subclinical episodes. There is, therefore, a need for prospective studies to determine whether this also influences the outcome.
The previously reported incidence of acute exacerbations of fibrosing IPs varies between 5 and 20 % [6, 25–27]. In many cases, “treatment” with high-dose corticosteroids (with or without an immunosuppressant) has proved ineffective and even fatal [27]. In addition, a study by Maldonado et al. [14] concluded that patients with more than 20 % iron-stain-positive macrophages in their BALF had a worse prognosis than those with less than 20 %, because they all died during hospitalization. However, data about coumarin use or other possible causes of DAH are lacking.
The strongest predictors of the variability of coumarin-induced anticoagulant effects in patients appeared to be genes encoding for the enzyme VKORC1; this enzyme was the target of vitamin K antagonists (Fig. 1). The enzyme VKORC1 reduces vitamin K epoxide to vitamin K, which after further reduction to the hydroquinone form is an essential cofactor in the formation of active vitamin K-dependent clotting factors [9]. Another predictor appears to be CYP2C9, the enzyme mainly responsible for the metabolism of coumarins. For instance, patients with the common, functionally defective, *2 (C430T) and *3 (A1075C) allelic variants of CYP2C9 require significantly lower maintenance doses, take longer to achieve dose stabilization, and are at higher risk for serious and life-threatening bleeding than patients without these variants [28]. Moreover, a previous study by Wijnen et al. [9] found that all but one of the included patients had at least one of these CYP2C9 or VKORC1 variant alleles, contributing to subsequent overshot international normalized ratios (INRs) and finally resulting in one or more episodes of DAH. Furthermore, patients bearing these VKORC1 and CYP2C9 polymorphisms appeared to have a significantly higher risk (almost 15 times higher than noncarriers of the variant alleles) of developing DAH and a possible ensuing fibrosing IP. This is why genotyping for these single nucleotide polymorphisms (SNPs) was recommended.
Vitamin K cycle. Carboxylation of certain glutamate (Glu) residues in proteins to gamma-carboxyglutamate (Gla) residues by vitamin K hydroquinone (KH2). Vitamin K epoxide (KO) is reduced to vitamin K (K) by vitamin K epoxide reductase complex 1 (VKORC1), which is inhibited by coumarin derivatives (anticoagulants), which in turn are metabolized by cytochrome 2C9 (CYP2C9)
It is tempting to speculate that an association with VKORC1 and/or CYP2C9 variant alleles might even be a risk factor for the development of fibrosing IP. Therefore, it is important to be informed about this allele status in individual patients as anticoagulant therapy is considered to offer added value in the therapeutic management of fibrosing IP patients [29]. Some studies into this matter were, however, subject to several methodological limitations and flaws, whereas others found no beneficial effect of anticoagulant therapy [3, 30, 31]. Also, a recent trial conducted with the goal to investigate the safety and efficacy of warfarin, using a double-blind, placebo-controlled design (ACE-IPF trial), found that treatment with warfarin offered no clinical benefit to patients with IPF and the agent even appeared to be harmful. Moreover, treatment with warfarin was associated with an increased risk of mortality due to respiratory worsening in a population of IPF patients who lacked other indications for anticoagulation. Based on these results, the investigators recommended that warfarin should not be used for the treatment of progressive IPF [32].
In addition, it has been emphasized that early recognition of the presence of one of the above-mentioned polymorphisms in DAH cases is important, in view of the potentially lethal outcome and the fact that simple vitamin K supplementation can be life-saving. Vitamin K supplementation is expected to diminish the inhibitory activity of coumarins and reduce the relative day-to-day variability of vitamin K intake and can significantly improve anticoagulation control in unstable patients [33, 34]. This vitamin K supplementation also can counteract the effect of low dietary uptake and/or antibiotic therapy [35–38]. Additionally, vitamin K can act as an antioxidant, reducing oxidative stress and NF-κB-dependent or -independent inflammation caused by the iron released during a DAH episode [7, 39, 40]. Whereas vitamin K is considered to be an antioxidant, its metabolites in the vitamin K cycle are classified as oxidants, especially vitamin K epoxide (KO) but also, although to a lesser degree, vitamin K hydroquinone (KH2; Fig. 1) [41, 42]. Tanaka et al. [43] also showed that vitamin K, more specifically vitamin K3, attenuated the severity of acute lung injury (ARDS) caused by the production of inflammatory mediators by immune cells, such as cytokines, chemokines, adhesion molecules, and bioactive lipid products.
A substantial and growing body of evidence indicates that oxidative stress is not only a pathological feature of fibrosing IP but that it is likely to play an important role in the development of fibrosis in multiple organ systems [8, 44, 45]. This has led to the suggestion that reactive oxygen species (ROS) are key players in the etiology of drug-induced lung damage [46]. This is supported by the observation that stimulators of ROS-generating enzymes, such as angiotensin II or endothelin, are initiators of pulmonary fibrosis [46]. Recently, it was found that ROS enter the lung fibroblast via chloride channels, which may then lead to the generation of transforming growth factor beta (TGF-β) and to the formation of collagen [47]. Redox cycling thus may be critically involved in the etiology of pulmonary fibrosis. Prescribing antioxidants therefore seems to be an additional therapeutic option to counteract the oxidative stress [48]. Vitamin K, its isoforms and metabolites, appear to be effective regulators of ROS generation and the redox system and have been used as anti-inflammatory agents [43]. Although only nine of our patients were receiving vitamin K supplementation, it appeared to be beneficial, avoiding unstable or overshot target INRs and avoiding repeated episodes of DAH as well as the resultant oxidative stress, and should therefore be considered. Pulmonary fibrosis is an end-stage disease and preventing it is preferable to curing it.
An effect similar to that described in the present manuscript, i.e., dependence on vitamin K metabolism, is not to be expected with other classes of anticoagulants, because they do not involve inhibition of vitamin K epoxide reductase. Heparin and its low molecular weight derivatives activate antithrombin, which inactivates thrombin and other proteases in the blood, and glycoprotein IIb/IIa receptor blockers do not affect vitamin K metabolism either [49–52].
Interestingly, there have been reports of cases of DAH in patients using heparin, as well as incidental reports in patients using glycoprotein IIb/IIa inhibitors [53, 54]. It would be interesting to study this in relation to pulmonary fibrosis.
Conclusions
Almost half of the patients with established episodes of DAH developed fibrosing IP; therefore, it seems that DAH might be a trigger in the development of fibrosing IP. This observation warrants prospective studies to further evaluate the clinical impact of these findings.
References
American Thoracic Society/European Respiratory Society (2002) International Multidisciplinary Consensus Classification of the Idiopathic Interstitial Pneumonias. This joint statement of the American Thoracic Society (ATS), and the European Respiratory Society (ERS) was adopted by the ATS board of directors, June 2001 and by the ERS Executive Committee, June 2001. Am J Respir Crit Care Med 165(2):277–304
Monaghan H, Wells AU, Colby TV, du Bois RM, Hansell DM, Nicholson AG (2004) Prognostic implications of histologic patterns in multiple surgical lung biopsies from patients with idiopathic interstitial pneumonias. Chest 125(2):522–526
Raghu G, Collard HR, Egan JJ et al (2011) An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med 183(6):788–824
Martinez FJ, Safrin S, Weycker D et al (2005) The clinical course of patients with idiopathic pulmonary fibrosis. Ann Intern Med 142(12 Pt 1):963–967
Churg A, Muller NL, Silva CI, Wright JL (2007) Acute exacerbation (acute lung injury of unknown cause) in UIP and other forms of fibrotic interstitial pneumonias. Am J Surg Pathol 31(2):277–284
Collard HR, Moore BB, Flaherty KR et al (2007) Acute exacerbations of idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 176(7):636–643
Rahman I, Skwarska E, Henry M, Davis M, O’Connor CM, FitzGerald MX, Greening A, MacNee W (1999) Systemic and pulmonary oxidative stress in idiopathic pulmonary fibrosis. Free Radic Biol Med 27(1–2):60–68
Markart P, Luboeinski T, Korfei M et al (2009) Alveolar oxidative stress is associated with elevated levels of nonenzymatic low-molecular-weight antioxidants in patients with different forms of chronic fibrosing interstitial lung diseases. Antioxid Redox Signal 11(2):227–240
Wijnen PA, Linssen CF, Haenen GR, Bekers O, Drent M (2010) Variant VKORC1 and CYP2C9 alleles in patients with diffuse alveolar hemorrhage caused by oral anticoagulants. Mol Diagn Ther 14(1):23–30
Balkisson R, Murray D, Hoffstein V (1992) Alveolar damage due to inhalation of amitrole-containing herbicide. Chest 101(4):1174–1176
Jinn Y, Akizuki N, Ohkouchi M, Inase N, Ichioka M, Marumo F (1998) Acute lung injury after inhalation of water-proofing spray while smoking a cigarette. Respiration 65(6):486–488
Kayser K, Plodziszewska M, Waitr E, Slodkowska J, Altiner M, Gabius HJ (1998) Diffuse pulmonary hemosiderosis after exposure to pesticides. A case report. Respiration 65(3):214–218
Spahr JE, Maul JS, Rodgers GM (2007) Superwarfarin poisoning: a report of two cases and review of the literature. Am J Hematol 82(7):656–660
Maldonado F, Parambil JG, Yi ES, Decker PA, Ryu JH (2009) Haemosiderin-laden macrophages in the bronchoalveolar lavage fluid of patients with diffuse alveolar damage. Eur Respir J 33(6):1361–1366
De Lassence A, Fleury-Feith J, Escudier E, Beaune J, Bernaudin JF, Cordonnier C (1995) Alveolar hemorrhage. Diagnostic criteria and results in 194 immunocompromised hosts. Am J Respir Crit Care Med 151(1):157–163
Hwang JH, Misumi S, Sahin H, Brown KK, Newell JD, Lynch DA (2009) Computed tomographic features of idiopathic fibrosing interstitial pneumonia: comparison with pulmonary fibrosis related to collagen vascular disease. J Comput Assist Tomogr 33(3):410–415
Quanjer PH, Tammeling GJ, Cotes JE, Pedersen OF, Peslin R, Yernault JC (1993) Lung volumes and forced ventilatory flows. Report working party standardization of lung function tests, European Community for steel and coal. Official statement of the European Respiratory Society. Eur Respir J Suppl 16:5–140
Jacobs JA, De Brauwer E (1999) BAL fluid cytology in the assessment of infectious lung disease. Hosp Med 60(8):550–555
Raghu G, Weycker D, Edelsberg J, Bradford WZ, Oster G (2006) Incidence and prevalence of idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 174(7):810–816
Gribbin J, Hubbard RB, Le Jeune I, Smith CJ, West J, Tata LJ (2006) Incidence and mortality of idiopathic pulmonary fibrosis and sarcoidosis in the UK. Thorax 61(11):980–985
Meltzer EB, Noble PW (2008) Idiopathic pulmonary fibrosis. Orphanet J Rare Dis 3:8
Kaarteenaho R, Kinnula VL (2011) Diffuse alveolar damage: a common phenomenon in progressive interstitial lung disorders. Pulm Med 531302:1–10
Navaratnam V, Fleming KM, West J, Smith CJ, Jenkins RG, Fogarty A, Hubbard RB (2011) The rising incidence of idiopathic pulmonary fibrosis in the UK. Thorax 66(6):462–467
Kim DS, Park JH, Park BK, Lee JS, Nicholson AG, Colby T (2006) Acute exacerbation of idiopathic pulmonary fibrosis: frequency and clinical features. Eur Respir J 27(1):143–150
Song JW, Hong SB, Lim CM, Koh Y, Kim DS (2011) Acute exacerbation of idiopathic pulmonary fibrosis: incidence, risk factors and outcome. Eur Respir J 37(2):356–363
Hyzy R, Huang S, Myers J, Flaherty K, Martinez F (2007) Acute exacerbation of idiopathic pulmonary fibrosis. Chest 132(5):1652–1658
Papiris SA, Manali ED, Kolilekas L, Kagouridis K, Triantafillidou C, Tsangaris I, Roussos C (2010) Clinical review: idiopathic pulmonary fibrosis acute exacerbations––unravelling Ariadne’s thread. Crit Care 14(6):246
Higashi MK, Veenstra DL, Kondo LM, Wittkowsky AK, Srinouanprachanh SL, Farin FM, Rettie AE (2002) Association between CYP2C9 genetic variants and anticoagulation-related outcomes during warfarin therapy. JAMA 287(13):1690–1698
Kubo H, Nakayama K, Yanai M, Suzuki T, Yamaya M, Watanabe M, Sasaki H (2005) Anticoagulant therapy for idiopathic pulmonary fibrosis. Chest 128(3):1475–1482
Brown KK, Wells AU (2008) Recent clinical trials in idiopathic pulmonary fibrosis and the BUILD-a study. Eur Respir J 17(109):116–122
Kinder BW, Collard HR, King TE Jr (2006) Anticoagulant therapy and idiopathic pulmonary fibrosis. Chest 130(1):302–303
Noth I, Anstrom KJ, Calvert SB, de Andrade J, Flaherty KR, Glazer C, Kaner RJ, Olman MA (2012) A placebo-controlled randomized trial of warfarin in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 186(1):88–95
Sconce E, Avery P, Wynne H, Kamali F (2007) Vitamin K supplementation can improve stability of anticoagulation for patients with unexplained variability in response to warfarin. Blood 109(6):2419–2423
Sconce EA, Avery PJ, Wynne HA, Kamali F (2008) Vitamin K epoxide reductase complex subunit 1 (VKORC1) polymorphism influences the anticoagulation response subsequent to vitamin K intake: a pilot study. J Thromb Haemost 6(7):1226–1228
Ferland G, Sadowski JA, O’Brien ME (1993) Dietary induced subclinical vitamin K deficiency in normal human subjects. J Clin Investig 91(4):1761–1768
Shimada K, Matsuda T, Inamatsu T, Urayama K (1984) Bleeding secondary to vitamin K deficiency in patients receiving parenteral cephem antibiotics. J Antimicrob Chemother 14(Suppl B):325–330
Ansell J, Hirsh J, Poller L, Bussey H, Jacobson A, Hylek E (2004) The pharmacology and management of the vitamin K antagonists: the seventh ACCP conference on antithrombotic and thrombolytic therapy. Chest 126(3 Suppl):204S–233S
Drent M, Wessels S, Jacobs JA, Thijssen H (2000) Association of diffuse alveolar haemorrhage with acquired vitamin K deficiency. Respiration 67(6):697
Rahman I, Biswas SK, Kirkham PA (2006) Regulation of inflammation and redox signaling by dietary polyphenols. Biochem Pharmacol 72(11):1439–1452
Vervoort LM, Ronden JE, Thijssen HH (1997) The potent antioxidant activity of the vitamin K cycle in microsomal lipid peroxidation. Biochem Pharmacol 54(8):871–876
Wu J, Chien CC, Yang LY, Huang GC, Cheng MC, Lin CT, Shen SC, Chen YC (2011) Vitamin K3–2, 3-epoxide induction of apoptosis with activation of ROS-dependent ERK and JNK protein phosphorylation in human glioma cells. Chem Biol Interact 193(1):3–11
Canfield LM, Davy LA, Thomas GL (1985) Anti-oxidant/pro-oxidant reactions of vitamin K. Biochem Biophys Res Commun 128(1):211–219
Tanaka S, Nishiumi S, Nishida M et al (2010) Vitamin K3 attenuates lipopolysaccharide-induced acute lung injury through inhibition of nuclear factor-kappaB activation. Clin Exp Immunol 160(2):283–292
Ding Q, Luckhardt T, Hecker L, Zhou Y, Liu G, Antony VB, de Andrade J, Thannickal VJ (2011) New insights into the pathogenesis and treatment of idiopathic pulmonary fibrosis. Drugs 71(8):981–1001
Kinnula VL, Fattman CL, Tan RJ, Oury TD (2005) Oxidative stress in pulmonary fibrosis: a possible role for redox modulatory therapy. Am J Respir Crit Care Med 172(4):417–422
Bast A, Weseler AR, Haenen GR, den Hartog GJ (2010) Oxidative stress and antioxidants in interstitial lung disease. Curr Opin Pulm Med 16(5):516–520
Qi S, den Hartog GJ, Bast A (2009) Superoxide radicals increase transforming growth factor-beta1 and collagen release from human lung fibroblasts via cellular influx through chloride channels. Toxicol Appl Pharmacol 237(1):111–118
Singal AK, Jampana SC, Weinman SA (2011) Antioxidants as therapeutic agents for liver disease. Liver Int 31(10):1432–1448
Denas G, Pengo V (2012) Current anticoagulant safety. Expert Opin Drug Saf 11(3):401–413
Costantino G, Ceriani E, Rusconi AM, Podda GM, Montano N, Duca P, Cattaneo M, Casazza G (2012) Bleeding risk during treatment of acute thrombotic events with subcutaneous LMWH compared to intravenous unfractionated heparin; a systematic review. PLoS One 7(9):e44553
Robert-Ebadi H, Le Gal G, Righini M (2009) Use of anticoagulants in elderly patients: practical recommendations. Clin Interv Aging 4:165–177
Steffel J, Luscher TF (2012) Vitamin K antagonists. Ready to be replaced? Hamostaseologie 32(4):249–257
Masip J, Vecilla F, Paez J (1998) Diffuse pulmonary hemorrhage after fibrinolytic therapy for acute myocardial infarction. Int J Cardiol 63(1):95–97
Awadh N, Ronco JJ, Bernstein V, Gilks B, Wilcox P (1994) Spontaneous pulmonary hemorrhage after thrombolytic therapy for acute myocardial infarction. Chest 106(5):1622–1624
Conflict of Interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wijnen, P.A., Verschakelen, J.A., Bast, A. et al. Diffuse Alveolar Hemorrhage in Coumarin Users: A Fibrosing Interstitial Pneumonia Trigger?. Lung 191, 53–59 (2013). https://doi.org/10.1007/s00408-012-9436-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-012-9436-2