Abstract
Background:
Reducing socioeconomic inequalities in lung cancer treatment may reduce survival inequalities. However, the reasons for treatment variation are unclear.
Methods:
Northern and Yorkshire cancer registry, Hospital Episode Statistics and lung cancer audit data sets were linked. Logistic regression was used to explore the role of stage, histology, performance status and comorbidity in socioeconomic inequalities in lung cancer treatment, for 28 733 lung cancer patients diagnosed in 2006–2010, and in a subgroup with stage recorded (n=7769, 27%).
Results:
Likelihood of receiving surgery was significantly lower in the most deprived group (odds ratio (OR)=0.75, 95% confidence interval (CI) 0.65–0.86); however, the OR was attenuated when including histological subtype (OR=0.82, 95% CI 0.71–0.96). Patients in the most deprived group were significantly less likely to receive chemotherapy in the fully adjusted full cohort model including performance status (OR=0.64, 95% CI 0.58–0.72) but not in the staged subgroup model when performance status was included (OR=0.88, 95% CI 0.72–1.08). Socioeconomic inequalities in radiotherapy were not found.
Interpretation:
Socioeconomic inequalities in performance status statistically explained socioeconomic inequalities in receipt of chemotherapy in the selective staged subgroup, but not in the full cohort. Socioeconomic variation in histological subtype may account for some of the socioeconomic inequalities in surgery.
Similar content being viewed by others
Main
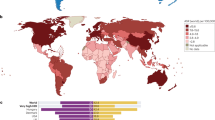
In England, less than 10% of those diagnosed with lung cancer survive for 5 years (Coleman et al, 2011). Lung cancer patients of lower socioeconomic position (SEP) have poorer survival (Rachet et al, 2010). It has been suggested that socioeconomic differences in receipt of cancer treatment might at least partially contribute to survival inequalities (Woods et al, 2006). There is some evidence that socioeconomic inequalities in lung cancer survival can be statistically explained by inequalities in treatment (Jack et al, 2006; Forrest et al, 2013b).
Socioeconomic inequalities in receipt of lung cancer surgery and chemotherapy, but not radiotherapy, were found in both universal (UHCS) and non-universal health-care systems, in a recent systematic review and meta-analysis (Forrest et al, 2013a). These findings could not be explained by the type of health-care system or by socioeconomic inequalities in stage at diagnosis. However, not all of the studies included in the review reported details of stage and histology, both of which influence treatment type (Forrest et al, 2013a), and very few took comorbidity into account. The review authors recommended that the reasons for socioeconomic inequalities in treatment should be more thoroughly investigated in studies including statistical control for comorbidity, stage and histology (Forrest et al, 2013a).
Performance status (PS), a global measure of functional status and an important consideration for clinicians treating lung cancer (NICE, 2005), is a factor that has not previously been well explored in studies examining socioeconomic inequalities in treatment. Although comorbidity and PS measure different things (the number of concurrent health conditions over a period of time before cancer diagnosis and general health status at the time of lung cancer diagnosis, respectively), both variables may be used as surrogate measures of suitability for treatment (Ludbrook et al, 2003). It is unclear how well comorbidity and PS capture fitness for treatment but, as the number of comorbidities varies by SEP for cancer patients (Louwman et al, 2010), this may help to explain inequalities in treatment.
Lung cancers are broadly classified into small cell (SCLC) and non-small cell (NSCLC) cancers, with NSCLC accounting for ∼80% of lung cancers. Non-small cell lung cancer can be further divided into squamous cell carcinoma, adenocarcinoma and large cell carcinoma subtypes (NICE, 2005). Squamous cell carcinoma is strongly associated with smoking, as is SCLC (Hirsch et al, 2008). Adenocarcinomas are a morphologically heterogeneous group and, although they are associated with smoking (Sharpe et al, 2012), they are also found in those who have never smoked, particularly in women (Hirsch et al, 2008). As SEP is associated with smoking and with histological subtype (Sharpe et al, 2012), histological subtype may confound the relationship between SEP and treatment for lung cancer.
In this study, we linked Northern and Yorkshire Cancer Registry and Information Centre (NYCRIS), Hospital Episode Statistics (HES) and National Lung Cancer Audit (LUCADA) data sets in order to examine the factors that may help to explain socioeconomic inequalities in lung cancer treatment (surgery, chemotherapy and radiotherapy). The role of stage, histology (and, within this, histological subtype), PS and comorbidity in statistically explaining socioeconomic inequalities in lung cancer treatment was specifically explored.
Materials and Methods
Data sources
The Northern and Yorkshire Cancer Registry is one of eight English regional cancer registries that collect a common minimum cancer data set (NYCRIS, 2012). Data on SEP, age, sex, histology, tumour, year of diagnosis, GP referral and details of receipt of treatment (surgery, chemotherapy and radiotherapy) were obtained from registry data. Comorbidity data were obtained from HES.
Incomplete recording of stage data is a major limitation of UK cancer registry data. However, stage data are collected by the LUCADA, a non-mandatory register of clinical information on patients diagnosed with lung cancer in the United Kingdom. The audit initially included only a subset of registry patients (66% nationally in 2006, increasing to 93% in 2010; NHS Information Centre, 2012).
Records were allocated a unique, randomly generated, key number, derived from the NHS number by NYCRIS. Data from the three data sources (NYCRIS cancer registry, HES and LUCADA data) were anonymised and supplied by NYCRIS. The HES and LUCADA data were then linked to the regional registry data using key numbers.
Variables of interest
Socioeconomic position was measured using the agreed methodology for all English cancer registries, the rank of the income domain of the Index of Multiple Deprivation (IMD). This is an area-based measure of SEP (HM Government, 2013), grouped into quintiles, where Q5 is the most deprived and Q1 the least deprived. The England-wide distribution of IMD was used. This is periodically updated to allow inclusion of the most recent data. The income domain of IMD2010 was used for patients diagnosed between 2007 and 2010. For those diagnosed in 2006 the income domain of IMD2007 was used.
Age at diagnosis was categorised into four groups: age <60, 60–69, 70–79 and 80+ years. Year of diagnosis was included to take into account changes in rates of treatment over time. GP referral was categorised as yes or no.
Lung cancer was categorised into the following eight histological subtypes: adenocarcinoma, large cell carcinoma, non-small cell carcinoma, squamous cell carcinoma, small cell carcinoma, other specified carcinoma, unspecified carcinoma (Riaz et al, 2012) and neoplasm. Lung cancer histology was classified as NSCLC, including adenocarcinoma, large cell carcinoma, non-small cell carcinoma and squamous cell carcinoma subtypes; SCLC; and other histology (including unspecified carcinoma, neoplasm and other specified carcinomas (including carcinoid tumours)), using ICD-0-3 morphology codes to categorise histological subtypes (WHO (World Health Organisation), 2000). When examining NSCLC and SCLC separately, the unspecified carcinoma and neoplasm subtypes were excluded and the other specified carcinoma subtype was included as probable NSCLC (Riaz et al, 2012).
A weighted comorbidity score was calculated by NYCRIS using the Charlson comorbidity index (CCI; Charlson et al, 1987) using the number of in-patient HES admissions for 16 specified conditions (excluding metastatic cancer) in the 3–18 months before diagnosis. HES-linked comorbidity data were not available for patients diagnosed in 2009–2010 as, because of national problems in calculating the comorbidity score, there was a time lag in data availability. Comorbidity score was categorised as 0, 1–2, 3+, missing or unavailable.
Stage and PS data were obtained from LUCADA. Stage was assigned using the TNM staging system (Sobin and Wittekind, 1997) and categorised as I, II, III, IV or missing. Performance status at the time of lung cancer diagnosis was recorded on a scale of 0 (asymptomatic) to 4 (bedridden) using the Eastern Cooperative Group PS scale (NICE, 2005) and categorised as 0, 1–2, 3–4 or missing.
Analysis
Data for 29 385 patients with a primary diagnosis of lung cancer (ICD10 C33 and C34), diagnosed between 1 January 2006 and 31 December 2010, were obtained. Of these, 652 had tumour registration based on death-certification only and were excluded from analyses, leaving an eligible cohort of 28 733.
The distribution of stage, histological subtype, PS and comorbidity by SEP was examined using χ2 tests. The distribution of each variable in the subgroup that had stage recorded (n=7769) was compared with that in the full cohort using χ2 tests to determine the representativeness of the subgroup.
Univariable and multivariable logistic regressions were used to examine the likelihood of receipt of each of three treatments – surgery, chemotherapy and radiotherapy, at any time after diagnosis – by SEP, in the full cohort and the staged subgroup. Receipt of surgery was also examined for probable NSCLC-only patients (n=16 278). Recipients of chemotherapy and radiotherapy were examined separately in probable NSCLC (n=16 278) and SCLC (n=3495) populations. Age, sex, histology (or histological subtype), year of diagnosis, GP referral, comorbidity, PS and stage (where available) were controlled for in fully adjusted models. A forward stepwise approach was used to explore which variables were important in explaining socioeconomic inequalities in treatment. The R2 statistic was examined as a measure of model fit, to determine the amount (%) of variance in receipt of treatment explained by each model. Odds ratios (ORs) with 95% confidence intervals (CIs) for the likelihood of receipt of treatment in each SEP quintile compared with the least deprived were reported. A likelihood ratio test was performed to determine the overall significance of each categorical variable. Analysis was carried out in Stata v12.0 (StataCorp, College Station, TX, USA).
Results
Table 1 shows the demographic and clinical characteristics of the cohort. Of the 28 733 patients included in the full cohort analysis, 7769 (27%) had stage and 8885 (31%) had a PS score recorded in LUCADA, and 8475 (29%) had a comorbidity score ascertained from HES. There were significant differences between the full cohort and the staged subgroup in the distribution of age group, histology, comorbidity and receipt of treatment, but not SEP or sex. The staged subgroups were younger, had a higher proportion of NSCLC patients and a higher proportion receiving treatment. Significant differences in distribution of PS, number of comorbidities and histology, but not stage at diagnosis, were seen by SEP. A higher proportion of more deprived patients had poor PS, more comorbidity and a squamous cell histological subtype (Supplementary Table 1).
Surgery
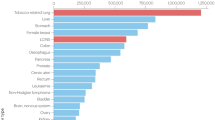
In the full cohort, the odds of receipt of surgery were significantly lower in the most compared to the least deprived group in the unadjusted analysis (OR=0.78, 95% CI 0.69–0.89) and in the fully adjusted multivariable analysis (OR=0.75, 95% CI 0.65–0.86). When histology was further broken down into histological subtypes then the SEP OR was attenuated (OR=0.82, 95% CI 0.71–0.96) (Table 2) and the amount of outcome variance explained by the model greatly increased (from R2=24.32% to 35.29%).
A similar result was seen for receipt of surgery in the most, compared with the least, deprived group in patients with probable NSCLC (OR=0.84, 95% CI 0.72–0.98; Supplementary Table 2), and in the subgroup that had stage recorded (OR=0.61, 95% CI 0.44–0.83; Supplementary Table 3).
Chemotherapy
Socioeconomic position was associated with receipt of chemotherapy in the fully adjusted full cohort model (OR=0.61, 95% CI 0.55–0.68). The inclusion of histological subtype rather than histology only marginally attenuated the odds ratio (OR=0.64, 95% CI 0.58–0.72; Table 3).
In the subgroup of patients who had stage recorded, no statistically significant association between SEP and receipt of chemotherapy was found in the unadjusted analysis (OR=0.86, 95% CI 0.73–1; Table 4) but was seen in a multivariable analysis including age, sex, histological subtype, year of diagnosis, GP referral, CCI score and stage (OR=0.73, 95% CI 0.60 to 0.88). However, on the addition of PS to the model the OR was attenuated and this association was no longer significant (OR=0.88, 95% CI 0.72–1.08; Table 4). Including PS also increased the model fit (R2=28.04% without PS, 35.86% with).
When chemotherapy was examined separately in probable NSCLC and SCLC populations, socioeconomic inequalities in receipt of chemotherapy were found for NSCLC (OR=0.67, 95% CI 0.59–0.76; Supplementary Table 4) and SCLC (OR=0.57, 95% CI 0.43–0.75; Supplementary Table 5). For NSCLC patients, the likelihood of chemotherapy increased over time but this was not seen for SCLC.
Radiotherapy
No association between SEP and receipt of radiotherapy was found in the full cohort in the fully adjusted model including histology (OR=1.03, CI 0.95–1.13) or histological subtype (OR=1.02, CI 0.93–1.11; Table 5). Similar results were found in the subgroup of patients who had stage recorded (OR=1.01, 95% CI 0.86–1.19). Different patterns of results were seen when receipt of radiotherapy was examined separately in probable NSCLC (OR=1.11, 95% CI 1–1.24) (Supplementary Table 6) and SCLC (OR=0.84, 95% CI 0.66–1.07; Supplementary Table 7) populations, but again were nonsignificant.
Discussion
Principal findings
This is one of the first UK registry-based studies to include a wide range of confounders and potentially important explanatory factors including stage, histology, comorbidity and PS, in order to determine their influence on socioeconomic inequalities in lung cancer treatment. In this study, we found socioeconomic inequalities in the receipt of surgery and chemotherapy, but not radiotherapy, for lung cancer, in the full cohort analyses. Having taken all the above factors into account, socioeconomic inequalities in receipt of surgery persisted. However, socioeconomic inequalities in receipt of chemotherapy were not found in the staged subgroup on addition of PS to the stepwise model.
Socioeconomic differences in PS statistically accounted for much of the socioeconomic inequality in receipt of chemotherapy in the staged subgroup. Socioeconomic differences in histological subtype may partially account for some of the observed socioeconomic differences in receipt of surgery observed.
Strengths and limitations
The use of multiple data set linkage (NYCRIS cancer registrations, HES and LUCADA) allowed us to include a broader range of potential confounders than previous UK registry studies (Jack et al, 2006; Berglund et al, 2012). Only two other UK studies (using early-year LUCADA audit data) have included PS in a multivariable analysis of receipt of lung cancer treatment (Rich et al, 2011a, 2011b). We were able to include later years of LUCADA data (2009–2010), which are more complete.
The population-based approach and the completeness and validity of the cancer registry data are the strengths of this study, although there may be some under-reporting of chemotherapy and radiotherapy treatments within registry data sets (Riaz et al, 2010). We used data from the north of England that may limit the generalisability of the findings to other locations. The high level of missing data for some variables is also a major limitation. Multiple imputation was considered but is not recommended, where over 50% of values for a variable are missing (White et al, 2011). To address the problem of missing data, we analysed complete-case data for the subset of patients who had stage recorded (the majority of whom also had PS recorded). As results from complete-case analyses can be biased (Sterne et al, 2009) we also analysed the full cohort and included missing categories for stage, PS and comorbidity, although this too can result in bias.
The validity of PS and CCI score as proxy measures of patients well-being is unclear. Performance status is a measure of patients acute functional status and need for care, assigned on a scale of 0–4 by the care team. Only moderate agreement in allocating PS score was found in an interobserver reliability study (Sorensen et al, 1993). However, there was good agreement when allocating good (PS 0–2) compared with poor PS (PS 3–4), which were similar to the groupings we employed.
The Charlson comorbidity index is a validated instrument for measuring comorbidity (Charlson et al, 1987) over a longer period of time. However, it may underestimate comorbidity as patients who suffer from a relevant condition but are treated entirely in primary care score zero. It has also been suggested that it is a crude measure of comorbidity, as patients with mild and severe forms of a disease receive the same score (Berglund et al, 2012). This could be a problem for conditions such as chronic pulmonary obstructive disease, where the severity of the disease is likely to influence the likelihood of receiving surgery for lung cancer. However, the index only contains details of conditions that are serious enough to require in-patient care.
Interpretation of results and comparison with other studies
Socioeconomic inequalities in receipt of surgery may be partially explained by socioeconomic differences in histological subtype. We found a significant association between SEP and histological subtype, with a lower proportion of squamous cell and higher proportion of adenocarcinoma subtype (and higher rates of treatment in this latter subtype) in the least deprived compared with most deprived group. A previous UK lung cancer study found that adenocarcinoma was less clearly associated with deprivation than other histological subtypes, possibly as it is less strongly associated with smoking (Bennett et al, 2008), and smoking is strongly socioeconomically patterned. It may be that health factors relating to smoking, rather than histological subtype, help to determine receipt of surgery, and we cannot rule out uncontrolled confounding related to smoking status. It is likely that smokers have generally poorer health and, although we were able to include PS and CCI score in the analysis, these measures may not fully capture this.
In agreement with the results from our systematic review of socioeconomic inequalities in lung cancer treatment (Forrest et al, 2013a), we found socioeconomic inequalities in receipt of surgery, and these remained after inclusion of stage, PS and comorbidity. In contrast, the only two other UK studies that included PS in a multivariable analysis of receipt of treatment, using national LUCADA data, found no association between SEP and receipt of surgery but did find an association with receipt of chemotherapy (Rich et al, 2011a, 2011b). We also found that, when including PS, SEP remained associated with a lower likelihood of receipt of chemotherapy in the full cohort but that SEP was no longer associated with receipt of chemotherapy in the staged subgroup.
The first few years of LUCADA data included only a small subset of registry patients and there were significant differences in stage at diagnosis, histology and PS when comparing patients from hospital Trusts with high levels of missing data with those who had low levels (Rich et al, 2011b). The validity of the pre-2007 LUCADA data has also been queried due to the poor entry of staging data (Murdoch et al, 2010). It may be that patients included in LUCADA in the early years of the audit are not representative of the full spectrum of patients diagnosed with lung cancer in England and this may explain the different pattern of results found using early audit data compared with studies using registry data. Concordance of recording of data on receipt of chemotherapy in LUCADA compared with registry data is reportedly poor, with 48% of patients with chemotherapy recorded in national registry data having no record of chemotherapy in LUCADA (Riaz et al, 2010); therefore, again this might account for some of the differences found.
Socioeconomic inequalities in receipt of radiotherapy were not found, although different patterns were seen for NSCLC compared with SCLC, when examined separately. It was not possible to distinguish between palliative and radical radiotherapy. Low-dose palliative radiotherapy is most commonly given, whereas fewer than 10% of patients receive high-dose radiotherapy with potentially curative intent. It is possible that differential effects by SEP might be seen if treatment-intent was examined, with more deprived SEP patients more likely to get palliative radiotherapy, and less deprived patients are likely to get curative radiotherapy. Potentially, these differential effects could effectively cancel each other out in statistical analyses and might help to explain why no overall association was found.
Implications for policy and practice
In this study, a higher percentage of more deprived patients had a squamous cell subtype that is strongly associated with smoking, although we were unable to measure smoking status in this cohort. Surgery rates were also lower for this histological subtype. Non-smokers are less likely to develop lung cancer and if they do then it may be that they are more likely to have a histological subtype that is more amenable to surgery. This is a further reason, if any other were required, to continue to promote aggressive antismoking and smoking-cessation campaigns.
The guidelines indicate that chemotherapy should be offered to stage III NSCLC patients and to stage IV patients with good PS (NICE, 2005). Socioeconomic differences in PS may determine whether a patient receives chemotherapy. Although there is a long chain of causality from health behaviours earlier in life to health status in later life, healthy behaviours should be encouraged, as patients who are in better health are likely to have a greater chance of receiving chemotherapy. It is unclear whether making lifestyle changes once diagnosed with cancer is likely to do much to improve PS, although a recent systematic review and meta-analysis produced preliminary evidence for improved survival for early-stage lung cancer patients who quit smoking after diagnosis (Parsons et al, 2010).
We were unable to take patient choice into account. Poorer health literacy may influence patient choice and understanding of risk, and this may vary by SEP (Protheroe et al, 2013), as might more fatalistic attitudes and health beliefs. If patients have poor capacity to process and understand basic health information, then they are less able to make appropriate health and treatment decisions (Nutbeam, 2008). It is important that clinicians take this into account when discussing treatment options.
Differences in communication patterns between health professionals and patients by SEP have been described that may influence the treatment prescribed (Murphy et al, 2010). Doctors may make treatment decisions based on which patients they consider likely to do well, using factors such as age, weight and comorbidity (Dixon-Woods et al, 2006) and these judgements may disadvantage more deprived lung cancer patients (Forrest, 2013). Treatment decisions should be clearly documented and should be based on the clinical guidelines.
Further research
The results from this study suggest that socioeconomic inequalities in PS statistically explain socioeconomic inequalities in receipt of chemotherapy in the subgroup of patients whose cancer was staged. However, this staged subgroup may not be representative of the full regional cohort as patients within this were more likely to be younger and to receive treatment. A previous study has shown a socioeconomic gradient in completeness of data on stage and grade of cancer, which could be interpreted as inequality in investigative intensiveness (Adams et al, 2004). It may be that younger patients receive more intensive investigation and so are more likely to be staged (Adams et al, 2004) and so, although PS may explain inequalities in chemotherapy in this group, they are a selective cohort. This is a relationship that needs to be clarified in other data sets, ideally with lower levels of missing data for stage and PS.
The observed relationship between histological subtype and receipt of surgery has not been consistently reported (Lüchtenborg et al, 2012) and further studies are also needed to confirm this association.
It would be useful to look at receipt of radiotherapy by curative or palliative intent to determine whether there are different patterns in likelihood of treatment by SEP.
Conclusions
Socioeconomic inequalities in lung cancer surgery and chemotherapy, but not in radiotherapy, were found. We have been able to investigate a number of factors that may be important in the relationship between SEP and receipt of treatment that have previously not been well explored; however, the high levels of missing data limit the conclusions that can be drawn.
Although histological subtype may account for some of the socioeconomic gradients in surgery, it does not explain it all. Socioeconomic inequalities in PS did not explain inequalities in chemotherapy in the full cohort analyses (although it did within the staged subgroup), and nor did stage or number of comorbidities, suggesting that other factors are responsible.
Further research is required to investigate the unexplained variance in treatment rates, exploring factors such as patient choice, doctor–patient communication of risk and benefit, and possible system variation by region, hospital and individual clinician.
Change history
29 July 2014
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Adams J, White M, Forman D (2004) Are there socioeconomic gradients in the quality of data held by UK cancer registries? J Epidemiol Community Health 58: 1052–1053.
Bennett V, Davies E, Jack R, Mak V, Moller H (2008) Histological subtype of lung cancer in relation to socio-economic deprivation in South East England. BMC Cancer 8 (1): 139.
Berglund A, Lambe M, Lüchtenborg M, Linklater K, Peake MD, Holmberg L, Møller H (2012) Social differences in lung cancer management and survival in South East England: a cohort study. BMJ Open 2 (3): e001048.
Charlson M, Pompei P, Ales K, MacKenzie C (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40: 373–383.
Coleman MP, Forman D, Bryant H, Butler J, Rachet B, Maringe C, Nur U, Tracey E, Coory M, Hatcher J, McGahan CE, Turner D, Marrett L, Gjerstorff ML, Johannesen TB, Adolfsson J, Lambe M, Lawrence G, Meechan D, Morris EJ, Middleton R, Steward J, Richards MA (2011) Cancer survival in Australia, Canada, Denmark, Norway, Sweden, and the UK, 1995-2007 (the International Cancer Benchmarking Partnership): an analysis of population-based cancer registry data. Lancet 377 (9760): 127–138.
Dixon-Woods M, Cavers D, Agarwal S, Annandale E, Arthur A, Harvey J, Hsu R, Katbamna S, Olsen R, Smith L, Riley R, Sutton A (2006) Conducting a critical interpretive synthesis of the literature on access to healthcare by vulnerable groups. BMC Med Res Methodol 6 (1): 35–47.
Forrest LF (2013) Why are socioeconomic inequalities in receipt of treatment found for lung cancer? Lung Cancer Manage 2 (3): 177–180.
Forrest LF, Adams J, Wareham H, Rubin G, White M (2013a) Socioeconomic inequalities in lung cancer treatment: systematic review and meta-analysis. PLoS Med 10 (2): e1001376.
Forrest LF, White M, Rubin G, Adams J (2013b) The effect of socioeconomic inequalities in receipt of, and time to, treatment on socioeconomic inequalities in lung cancer survival: an observational, data-linkage study. Lancet 382: S37.
Hirsch FR, Spreafico A, Novello S, Wood MD, Simms L, Papotti M (2008) The prognostic and predictive role of histology in advanced non-small cell lung cancer: a literature review. J Thorac Oncol 3 (12): 1468–1481.
HM Government (2013) English Indices of Deprivation 2010.
Jack RH, Gulliford MC, Ferguson J, Møller H (2006) Explaining inequalities in access to treatment in lung cancer. J Eval Clin Pract 12 (5): 573–582.
Louwman WJ, Aarts MJ, Houterman S, van Lenthe FJ, Coebergh JWW, Janssen-Heijnen MLG (2010) A 50% higher prevalence of life-shortening chronic conditions among cancer patients with low socioeconomic status. Br J Cancer 103 (11): 1742–1748.
Lüchtenborg M, Jakobsen E, Krasnik M, Linklater KM, Mellemgaard A, Møller H (2012) The effect of comorbidity on stage-specific survival in resected non-small cell lung cancer patients. Eur J Cancer 48 (18): 3386–3395.
Ludbrook JJS, Truong PT, MacNeil MV, Lesperance M, Webber A, Joe H, Martins H, Lim J (2003) Do age and comorbidity impact treatment allocation and outcomes in limited stage small-cell lung cancer? A community-based population analysis. Int J Radiat Oncol Biol Phys 55 (5): 1321–1330.
Murdoch C, Wilkinson J, Unsworth L (2010) Lung resection rates across the North of England Cancer Network Available at http://www.nepho.org.uk/publications.php5?rid=823.
Murphy MM, Tseng JF, Shah SA (2010) Disparities in cancer care: an operative perspective. Surgery 147 (5): 733–737.
NHS Information Centre (2012) National Lung Cancer Audit Report 2012. Leeds: NHS Information Centre for Health and Social Care. Available at www.hqip.org.uk/.../Lung-Cancer-National-Audit-Report-pub-2012.pdf.
NICE (2005) Clinical Guideline 24. Lung Cancer: the Diagnosis and Treatment of Lung Cancer. NICE: London.
Nutbeam D (2008) The evolving concept of health literacy. Soc Sci Med 67 (12): 2072–2078.
NYCRIS (2012) Northern and Yorkshire Cancer Registry and Information Centre. Available at http://www.nycris.nhs.uk/about/ . Accessed on 02 August 2013.
Parsons A, Daley A, Begh R, Aveyard P (2010) Influence of smoking cessation after diagnosis of early stage lung cancer on prognosis: systematic review of observational studies with meta-analysis. Br Med J 340: b5569.
Protheroe J, Brooks H, Chew-Graham C, Gardner C, Rogers A (2013) Permission to participate? A qualitative study of participation in patients from differing socio-economic backgrounds. J Health Psychol 18 (8): 1046–1055.
Rachet B, Ellis L, Maringe C, Chu T, Nur U, Quaresma M, Shah A, Walters S, Woods L, Forman D, Coleman MP (2010) Socioeconomic inequalities in cancer survival in England after the NHS cancer plan. Br J Cancer 103 (4): 446–453.
Riaz SP, Linklater K, Horton M, Peake M, Moller H, Luchtenborg M (2010) Lung cancer data in the National Cancer Data Repository, Hospital Episode Statistics and National Lung Cancer Audit datasets. Available at www.ncin.org.uk/view?rid=1624.
Riaz SP, Lüchtenborg M, Coupland VH, Spicer J, Peake MD, Møller H (2012) Trends in incidence of small cell lung cancer and all lung cancer. Lung Cancer 75 (3): 280–284.
Rich AL, Tata LJ, Free CM, Stanley RA, Peake MD, Baldwin DR, Hubbard RB (2011a) Inequalities in outcomes for non-small cell lung cancer: the influence of clinical characteristics and features of the local lung cancer service. Thorax 66 (12): 1078–1084.
Rich AL, Tata LJ, Stanley RA, Free CM, Peake MD, Baldwin DR, Hubbard RB (2011b) Lung cancer in England: Information from the National Lung Cancer Audit (LUCADA). Lung Cancer 72 (1): 16–22.
Sharpe KH, McMahon AD, McClements P, Watling C, Brewster DH, Conway DI (2012) Socioeconomic inequalities in incidence of lung and upper aero-digestive tract cancer by age, tumour subtype and sex: a population-based study in Scotland (2000–2007). Cancer Epidemiol 36 (3): e164–e170.
Sobin LH, Wittekind CH (1997) TNM Classification of Malignant Tumors 5th edn John Wiley & Sons: New York, NY, USA.
Sorensen J, Klee M, Palshof T, Hansen H (1993) Performance status in cancer patients. An inter-observer variability study. Br J Cancer 67: 773–775.
Sterne JA, White IR, Carlin JB, Spratt M, Royston P, Kenward MG, Wood AM, Carpenter JR (2009) Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. Br Med J 338: b2393.
White IR, Royston P, Wood AM (2011) Multiple imputation using chained equations: issues and guidance for practice. Stat Med 30 (4): 377–399.
WHO (World Health Organisation) (2000) International Classification of Diseases for Oncology (3rd (ICD-0-3)) (Accessed on 30 April 2014).
Woods LM, Rachet B, Coleman MP (2006) Origins of socio-economic inequalities in cancer survival: a review. Ann Oncol 17 (1): 5–19.
Acknowledgements
LFF was funded by the ESRC (PhD studentship ES/I020926/1) as a member of Fuse, the Centre for Translational Research in Public Health (www.fuse.ac.uk). MW is director, GR a senior investigator and JA is funded as a staff member of Fuse. Fuse is a UK Clinical Research Collaboration (UKCRC) Public Health Research Centre of Excellence. We acknowledge the funding for Fuse from the British Heart Foundation, Cancer Research UK, Economic and Social Research Council, Medical Research Council, the National Institute for Health Research, under the auspices of the UKCRC. We would like to thank staff at NYCRIS for extracting and supplying the data for linkage.
Author Contributions
LFF designed the study, obtained the data, conducted the analysis and wrote the first draft of the manuscript. JA, MW and GR had the initial idea for the study, obtained the funding, and were involved in data interpretation and critical revision of the manuscript. The final manuscript was approved by all authors before submission. All authors will act as guarantor.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Disclaimer
The views expressed in this paper do not necessarily represent those of the funders or UKCRC. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Ethical Approval
Ethical Approval was applied for through the Integrated Research Application System (IRAS) for NHS Research Ethics Committee (REC) approval. A favourable ethical opinion was obtained from the Proportionate Review subcommittee of the NRES Committee East of England REC on the 13 December 2011 (REC reference 11/EE/0537).
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Supplementary Information accompanies this paper on British Journal of Cancer website
Supplementary information
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Forrest, L., White, M., Rubin, G. et al. The role of patient, tumour and system factors in socioeconomic inequalities in lung cancer treatment: population-based study. Br J Cancer 111, 608–618 (2014). https://doi.org/10.1038/bjc.2014.310
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2014.310
Keywords
This article is cited by
-
Are socio-economic inequalities in breast cancer survival explained by peri-diagnostic factors?
BMC Cancer (2021)
-
A systematic review and meta-analysis of haematological malignancies in residents living near petrochemical facilities
Environmental Health (2020)
-
The effect of socioeconomic status on health-care delay and treatment of esophageal cancer
Journal of Translational Medicine (2015)
-
Factors associated with timeliness of post-primary care referral, diagnosis and treatment for lung cancer: population-based, data-linkage study
British Journal of Cancer (2014)