Abstract
Objective
To evaluate the impact of continuous subglottic suctioning and semi-recumbent body position on bacterial colonisation of the lower respiratory tract.
Design
A randomised controlled trial.
Setting
The ten-bed medical ICU of a French university hospital.
Patients
Critically ill patients expected to require mechanical ventilation for more than 5 days.
Interventions
Patients were randomly assigned to receive either continuous suctioning of subglottic secretions and semi-recumbent body position or to receive standard care and supine position.
Measurements and results
Oropharyngeal and tracheal secretions were sampled daily and quantitatively cultured. All included patients were followed up from day 1 (intubation) to day 10, extubation or death. Ninety-seven samples of oropharynx and trachea were analysed (40 for the suctioning group and 57 for the control group). The median bacterial counts in trachea were 6.6 Log10 CFU/ml (interquartile range, IQR, 4.4–8.3) in patients who received continuous suctioning and 5.1 Log10 CFU/ml (IQR 3.6–5.5) in control patients. Most of the patients were colonised in the trachea after 1 day of mechanical ventilation (75% in the suctioning group, 80% in the control group). No significant difference was found in the daily bacterial counts in the oropharynx and in the trachea between the two groups of patients.
Conclusion
Tracheal colonisation in long-term mechanically ventilated ICU patients was not modified by the use of continuous subglottic suctioning and semi-recumbent body position.
Similar content being viewed by others
Introduction
Nosocomial pneumonia associated with mechanical ventilation (VAP) remains of great concern in critically ill patients because of its high incidence and significant impact on outcome in terms of excess morbidity and mortality [1, 2]. Therefore, new strategies of prevention must be devised and evaluated in order to reduce the occurrence of these severe infections [3, 4, 5, 6]. The most commonly recognised cause of nosocomial pneumonia, the so-called “gastro-pulmonary hypothesis”, is tracheal colonisation by oropharynx and/or gastric flora leading to subsequent aspiration of oropharyngeal contents into the lower airways [7, 8]. Recently, two mechanical methods were proposed to escape this pathogenic mechanism. The first consists of placing ventilated patients in a semi-recumbent body position to limit regurgitation of gastric contents, the second of using endotracheal tubes modified to permit continuous subglottic suctioning of oropharyngeal secretions. Both methods have been shown to decrease the incidence of VAP in randomised controlled trials [9, 10, 11, 12, 13]. Moreover, despite a higher cost as compared to standard endotracheal tubes, the use of subglottic suctioning may result in savings as reported in a cost-benefit analysis [14]. The concept of continuous subglottic suctioning is based on the assumption that reducing aspiration of bacteria pooled above the cuff of the endotracheal tube into the lower respiratory tract decreases the risk of VAP. Clinical trials evaluating subglottic suctioning have focused on the prevention of early-onset pneumonia. The aim of our study was to assess whether the use of continuous subglottic suctioning and semi-recumbent body position reduces the bacterial burden in the trachea of long-term ventilated patients.
Patients and methods
Patients
Critically ill ventilated patients, hospitalised in the ten-bed medical ICU of Broussais university hospital and expected at admission to require mechanical ventilation for more than 5 days, were eligible for the study and randomly assigned to one of two groups. We chose a minimum of 5 days in order to monitor the impact of suctioning on long-term tracheal colonisation. Indeed, subglottic suctioning could either delay tracheal colonisation or secondarily reduce its level. Patients were randomised immediately before intubation. The suctioning group included patients intubated in the ICU with an endotracheal tube with a separate dorsal lumen ending in the subglottic area for continuous suctioning of secretions in the space above the cuff (HI-LO Evac; Mallinckrodt Laboratories, Athlone, Ireland). Patients of this group were also placed in semi-recumbent position (30°) in the bed. The control group was composed of patients intubated in the ICU with a standard endotracheal tube and placed in supine position in the bed. Patients were excluded if they had been intubated within the 15 days preceding ICU admission.
The monitoring period extended from day 1 (intubation) to day 10, extubation, onset of VAP or death. No selective decontamination regimen or antibiotic prophylaxis was used. All patients received sucralfate for stress ulcer prophylaxis. Tracheal cuff pressure was monitored at least three times a day with the aim of pressure between 20 and 30 mmHg [15]. The permeability of the drainage system was monitored every 4 h. The level of aspiration of the drainage system was −30 mmHg. The daily amount of subglottic secretions aspirated was not monitored because of its extreme variability from one patient to another and its dependence on many factors including the volume of oropharyngeal secretion, the volume of gastro-oesophageal secretions and the modalities of oropharyngeal care. The institution’s clinical investigation committee approved the study protocol.
Data collection and definitions
Each patient’s demographic characteristics, primary diagnosis, underlying diseases, reason for mechanical ventilation, previous pneumonia and previous antibiotic therapy were prospectively recorded. Indices measuring the severity of illness (Acute Physiology And Chronic Health Evaluation, APACHE II, score) [16], the number of organ dysfunctions (organ dysfunctions and infection, ODIN score) [17], the neurological status (Glasgow coma scale) [18] and the therapeutic activity (Therapeutic Intervention Scoring System, TISS) [19] were calculated on day 1.
Colonisation of the oropharynx or the trachea was defined by the presence of the same organisms on at least two successive samples, in the absence of infection. VAP was suspected in patients who met the following criteria: fever, (body temperature ≥38.3°C), leukocytosis (>12,000 leukocytes/mm3), macroscopically purulent tracheal secretions and the presence of new and persistent lung infiltrates on chest roentgenogram. These patients underwent fibre optic bronchoscopy and the diagnosis of VAP was ascertained by a positive protected specimen brush culture containing at least one micro-organism recovered at a significant concentration and/or a positive direct examination of bronchoalveolar lavage fluid with more than 5% of cells containing intracellular bacteria [20, 21, 22].
Bacteriological examination
Surveillance quantitative cultures for aerobic and anaerobic micro-organisms of both the oropharyngeal and tracheal secretions were obtained daily from all patients during the study period. An aliquot of 0.1 ml of oropharyngeal and tracheal secretions was isolated on Colombia agar plates supplemented with 5% horse blood for aerobic and anaerobic cultures. Serial tenfold dilutions (10−1 to 10−6) were made and 0.1 ml aliquots of each specimen; each dilution was placed on a chocolate agar plate supplemented with Isovitalex (BD Mérieux, France) and incubated under 10% CO2. Global as well as individual species bacterial counts were determined after 18 h of incubation at 37°C. Bacterial identification and susceptibility testing were performed using Api system (BD Mérieux, France) as well as standard methods [23].
End points
First, the effect of continuous subglottic drainage and semi-recumbent position was evaluated by measuring the bacterial counts harboured in the trachea and oropharynx of the patients. Second, bacterial counts recovered in the oropharynx and in the trachea were measured daily. Thus, the time course of colonisation between the two groups of patients was compared quantitatively.
Statistical analysis
Bacterial counts were expressed as log10 transformed number of CFU per millilitre of secretions. The average bacterial count for each patient was obtained by calculating the median over the samplings and a Mann-Whitney test was used to compare the bacterial counts of the two groups. In patients who developed VAP and received antimicrobial treatment, only bacterial counts prior to the occurrence of infection were included in the analysis. Summary statistics on log10 transformed bacterial counts were expressed as means ± SD, medians and interquartile ranges. The chi-square test or Fisher’s exact test was used for categorical variables expressed as percentage. Statistica 4.5 (Statsoft, Tulsa, OK) was used to perform the analysis. All p values were two-tailed, with significance set at 0.05.
Results
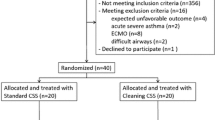
According to the flow diagram shown in Fig. 1, 104 patients were intubated in the unit and 18 patients were actually included in the study. Eight patients were randomly assigned to receive continuous suctioning of subglottic secretions and ten had a standard endotracheal tube. The two groups were similar for demographic characteristics, primary diagnosis and underlying diseases (Table 1). The median duration of follow-up was 10 days (IQR 7–10 days) for the suctioning group and 8 days (IQR 5–9 days) for the control group. The median duration of mechanical ventilation was 12 days in the two groups with an interquartile range of 5–14 days in the suctioning group and 7–15 days in the control group.
During the study protocol, 120 paired cultures of oropharynx and trachea samples were performed and 97 analysed: 40 for the suctioning group and 57 for the control group. The overall comparison of quantitative colonisation data between the two groups is reported in Table 2. In the suctioning group, 75% of patients were colonised in the trachea after 1 day of mechanical ventilation compared to 80% in the control group. Overall, bacterial counts in the oropharynx and the trachea did not differ significantly between the two groups. The differences obtained between the last and the first samples in the trachea per patient are shown in Fig. 2. Tracheal colonisation decreased in four of ten (40%) patients randomised in the control group versus three of eight (38%) patients in the suctioning group. Tracheal bacterial burden reached 106 CFU/ml in all patients, except one in the suctioning group, with a median time lapse after intubation of 1 day and 2 days for the suctioning and control groups, respectively. Fig. 3 shows the kinetics of colonisation during monitoring. No significant difference was found in the daily bacterial counts in the oropharynx and in the trachea between the two groups of patients. The relationships between bacterial counts simultaneously recovered in the oropharynx and in the trachea are shown in Fig. 4. Graphically, the shapes of the scatter plots appeared similar in the two groups. Since counts were not independent, no statistical test was performed. The micro-organisms recovered from the daily surveillance cultures are listed in Table 3.
Time course of tracheal and oropharyngeal colonisation in patients assigned to continuous subglottic suctioning and semi-recumbent position (solid squares) and patients assigned to standard endotracheal tube and supine position (open diamonds). No significant difference was found in daily bacterial counts between the two groups of patients
Seven episodes of VAP occurred in five patients of the suctioning group compared to six episodes in six control patients, with median time-lapses of 4 days and 12 days, respectively. First episodes involved in most cases: Pseudomonas aeruginosa (1 in the suctioning group and 2 in the control group); Staphylococcus aureus (3 and 1, respectively) and enterobacteria (2 and 3, respectively). In five (45%) patients who acquired VAP, the micro-organisms involved were “new” colonisers not present at baseline (2 in the suctioning group and 3 in the control group). Among the five patients who were extubated in the suctioning group, two (40%) developed laryngeal oedema immediately after extubation. No other adverse effects were observed.
Discussion
The main finding of this randomised controlled trial suggests that the use of continuous subglottic suctioning and semi-recumbent position did not modify the level of oropharyngeal and tracheal colonisation in long-term ventilated critically ill patients, nor appear to influence the kinetics of colonisation.
One may argue that the size of the study population was too small to see any difference. However, the main end point was not to assess VAP rate in patients, but to compare simultaneous cultures of oropharyngeal and tracheal specimens (40 pairs in the suctioning group and 57 pairs in the control group), since it is the main physiopathological pathway for VAP, which can be influenced by subglottic suctioning and semi-recumbent body position. Although this study was not powered enough to detect differences in the rate of nosocomial pneumonia, the hypothesis was to detect a difference in the rates of colonisation between the two groups.
To date, four randomised trials have evaluated whether the use of an endotracheal tube allowing continuous drainage of subglottic secretions via a separate lumen above the cuff reduced the risk of VAP in ICU patients [10, 11, 12, 13]. The main design characteristic of these trials was to focus on the prevention of pneumonia during the first 5–7 days of mechanical ventilation. Mahul et al. compared 70 patients receiving intermittent (hourly) subglottic secretion drainage to 75 patients intubated with a standard endotracheal tube and found a significantly lower incidence of VAP in the group with subglottic suctioning (13 versus 29%) and a beneficial effect on tracheal colonisation rates [10]. Interestingly, they gave the respective distributions of colonised and non-colonised patients in the two groups at entry into the study. It is noteworthy that when one removes non-colonised patients from the analysis, VAP rates did not remain significantly different between the two groups (3/15, 20% versus 6/21, 29%, p=0.55).
In another trial, the observed reduction of the VAP rates with subglottic drainage did not reach statistical significance, although the incidence density was lower; however, Valles et al. did not clearly indicate whether patients had tracheal colonisation on admission [11]. More than half of the patients in that study were comatose or had chronic obstructive pulmonary disease, which are conditions well known to favour tracheal colonisation and to predispose to nosocomial pneumonia [24, 25]. Kollef et al. reported the results of a randomised clinical trial conducted in 343 patients admitted to a cardiothoracic surgical ICU [12]. Even though VAP rates were similar in patients with continuous subglottic suctioning and patients without suctioning, the occurrence of VAP was significantly delayed in patients receiving continuous drainage. No data were shown regarding initial colonisation of the patients’ upper airways. Recently, Smulders et al. evaluated the impact of intermittent subglottic suctioning in patients ventilated for more than 72 h [13]. VAP rates were significantly lower in patients receiving intermittent subglottic suctioning than in patients receiving standard endotracheal tube. No mention was made of tracheal colonisation.
In our study, most patients had heavily colonised trachea from the first day of the protocol. Moreover, only patients expected to require mechanical ventilation for more than 5 days were eligible for the study. This led to the enrolling of mainly patients with long-term ventilator-dependency, which may explain why we were unable to see any reduction in the tracheal colonisation rate in patients receiving continuous subglottic suctioning and semi-recumbent body position. Actually, it is possible that prior heavy tracheal colonisation constitutes a factor limiting the effectiveness of these measures to reduce micro-aspirations of contaminated secretions into the lower airways. When a high level of tracheal colonisation pre-existed, the intervention failed to decrease bacterial counts during its use. This is all the more important since a large percentage of patients (generally more than 50%) are already colonised in the oropharynx and the trachea when admitted to the ICU [24, 25, 26, 27, 28, 29]. In addition, the higher the concentration of micro-organisms colonising the pharyngeal region, the greater the risk of colonisation of the lower airways [26]. Therefore, subglottic suctioning might be relevant in certain subgroups of patients not heavily colonised in the trachea to prevent early-onset VAP.
Another limitation of our study may be that all patients received stress ulcer prophylaxis with sucralfate that may have had some influence on colonisation. Since gastric colonisation was not studied, inferences on this point are limited.
Semi-recumbency has been shown to prevent the occurrence of VAP, probably by protecting the patient from pulmonary aspiration [9, 30]. Orozco-Levi et al. also demonstrated that semi-recumbent positioning did not protect completely from gastro-oesophageal reflux and subsequently from oropharyngeal colonisation from gastric origin in mechanically ventilated patients [30]. Moreover, positioning patients at a 30° trunk flexion is not so easy to implement in routine practice and clinical estimates of trunk position may be not accurate [31]. Since semi-recumbency positioning was based on clinical estimation, we cannot be sure that patients’ trunk flexions were set accurately and continually at a 30° angle. Another hypothesis is that a 30° angle may not be sufficient to achieve aspiration prevention and semi-recumbency should be set at 45° [9].
The specific design of our study, combining two interventions, might have masked any preventive effect of one or the other method. One recent experimental study evaluated the effects on tracheal colonisation of continuous subglottic suctioning in two groups of sheep with different head orientations (head elevated at a 30° angle above horizontal or head flat or below horizontal) [32]. The trachea and lungs of all sheep with head up were heavily colonised, which is consistent with the results of our study.
The routine implementation of continuous subglottic suctioning was sometimes demanding in terms of nursing workload (i.e., maintaining continuous drainage, ensuring proper position of the endotracheal tube and setting the appropriate cuff pressure to prevent leakage of contaminated secretions into the lower airway) [6, 32]. Furthermore, in patients under continuous suctioning, some adverse effects were observed; 40% of the patients developed laryngeal oedema leading to reintubation whereas the overall rate of these complications is known to vary from 2–7% of extubations [33, 34]. Berra et al. showed that, at autopsy, all sheep exhibited tracheal mucosal injury (erythema, haemorrhage, necrosis) at the level of the evacuation port of the Hi-Lo Evac endotracheal tube [32]. Smulders et al. chose intermittent instead of continuous subglottic suctioning because of the risk of damaging the tracheal wall [13].
In conclusion, continuous subglottic suctioning and semi-recumbent position did not reduce tracheal colonisation in long-term ventilated patients.
References
Craven DE, Steger KA (1995) Epidemiology of nosocomial pneumonia. New perspectives on an old disease. Chest 108 (Suppl. 2):1S–16S
Fagon JY (1997) Influence of pneumonia on the mortality of the critically ill. Curr Opin Crit Care 3:56–64
American Thoracic Society (1996) Hospital-acquired pneumonia in adults: diagnosis, assessment of severity, initial antimicrobial therapy and preventive strategies. A consensus statement. Am J Respir Crit Care Med 153:1711–1725
Tablan OC, Anderson LJ, Arden NH, Breiman RF, Butler JC, McNeil MM (1994) Guideline for prevention of nosocomial pneumonia. The Hospital Infection Control Practices Advisory Committee, Centers for Disease Control and Prevention. Infect Control Hosp Epidemiol 15:587–627
Cook D, De Jonghe B, Brochard L, Brun-Buisson C (1998) Influence of airway management on ventilator-associated pneumonia. JAMA 279:781–787
Kollef MH (1999) The prevention of ventilator-associated pneumonia. N Engl J Med 340:627–634
Estes RJ, Meduri GU (1995) The pathogenesis of ventilator-associated pneumonia: I. Mechanisms of bacterial transcolonization and airway inoculation. Intensive Care Med 21:365–383
Niederman MS, Craven DE (1997) Editorial response: Devising strategies for preventing nosocomial pneumonia—should we ignore the stomach? Clin Infect Dis 24:320–323
Drakulovic MB, Torres A, Bauer TT, Nicolas JM, Nogue S, Ferrer M (1999) Supine body position as a risk factor for nosocomial pneumonia in mechanically ventilated patients: a randomised trial. Lancet 354:1851–1858
Valles J, Artigas A, Rello J, Bonsoms N, Fontanals D, Blanch L, Fernandez R, Baigorri F, Mestre J (1995) Continuous aspiration of subglottic secretions in preventing ventilator-associated pneumonia. Ann Intern Med 122:179–186
Mahul P, Auboyer C, Jospe R, Ros A, Guerin C, el Khouri Z, Galliez M, Dumont A, Gaudin O (1992) Prevention of nosocomial pneumonia in intubated patients: respective role of mechanical subglottic secretions drainage and stress ulcer prophylaxis. Intensive Care Med 18:20–25
Kollef MH, Skubas NJ, Sundt TM (1999) A randomized clinical trial of continuous aspiration of subglottic secretions in cardiac surgery patients. Chest 116:1339–1346
Smulders K, van der Hoeven H, Weers-Pothoff I, Vandenbroucke-Grauls C (2002) A randomized clinical trial of intermittent subglottic secretion drainage in patients receiving mechanical ventilation. Chest 121:858–862
Shorr AF, O’Malley PG (2001) Continuous subglottic suctioning for the prevention of ventilator-associated pneumonia. Potential economic implications. Chest 119:228–235
Stauffer JL (1994) Complications of translaryngeal intubation. In: Tobin MJ (ed) Principles and practice of mechanical ventilation. McGraw-Hill, New York, p 740
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) APACHE II: a severity of disease classification system. Crit Care Med 13:818–829
Fagon JY, Chastre J, Novara A, Medioni P, Gibert C (1993) Characterization of intensive care unit patients using a model based on the presence or absence of organ dysfunctions and/or infection: the ODIN model. Intensive Care Med 19:137–144
Teasdale G, Jennett B (1974) Assessment of coma and impaired consciousness. A practical scale. Lancet 2:81–84
Cullen DJ, Civetta JM, Briggs BA, Ferrara LC (1974) Therapeutic intervention scoring system: a method for quantitative comparison of patient care. Crit Care Med 2:57–61
Chastre J, Fagon JY, Soler P, Bornet M, Domart Y, Trouillet JL, Gibert C, Hance AJ (1988) Diagnosis of nosocomial bacterial pneumonia in intubated patients undergoing ventilation: comparison of the usefulness of bronchoalveolar lavage and the protected specimen brush. Am J Med 85:499–506
Wimberley N, Faling LJ, Bartlett JG (1979) A fiberoptic bronchoscopy technique to obtain uncontaminated lower airway secretions for bacterial culture. Am Rev Respir Dis 119:337–343
Fagon JY, Chastre J, Hance AJ, Guiguet M, Trouillet JL, Domart Y, Pierre J, Gibert C (1988) Detection of nosocomial lung infection in ventilated patients. Use of a protected specimen brush and quantitative culture techniques in 147 patients. Am Rev Respir Dis 138:110–116
Lennette EH, Balows A, Hausler WJJ, Truland JP (1980) Manual of clinical microbiology. 3rd edn. American Society of Microbiology, Washington, DC
Ewig S, Torres A, El-Ebiary M, Fabregas N, Hernandez C, Gonzalez J, Nicolas JM, Soto L (1999) Bacterial colonization patterns in mechanically ventilated patients with traumatic and medical head injury. Incidence, risk factors and association with ventilator-associated pneumonia. Am J Respir Crit Care Med 159:188–198
Zalacain R, Sobradillo V, Amilibia J, Barron J, Achotegui V, Pijoan JI, Llorente JL (1999) Predisposing factors to bacterial colonization in chronic obstructive pulmonary disease. Eur Respir J 3:343–348
Bonten MJM, Gaillard CA, van Tiel FH, Smeets HGW, van der Geest S, Stobberingh EE (1994) The stomach is not a source for colonization of the upper respiratory tract and pneumonia in ICU patients. Chest 105:878–884
Garrouste-Orgeas M, Chevret S, Arlet G, Marie O, Rouveau M, Popoff N, Schlemmer B (1997) Oropharyngeal or gastric colonization and nosocomial pneumonia in adult intensive care unit patients. Am J Respir Crit Care Med 56:1647–1655
Van Uffelen R, van Saene HKF, Fidler V, Löwenberg A (1984) Oropharyngeal flora as a source of bacteria colonizing the lower airways in patients on artificial ventilation. Intensive Care Med 10:233–237
De Latorre FJ, Pont T, Ferrer A, Rossello J, Palomar M, Planas M (1995) Pattern of tracheal colonization during mechanical ventilation. Am J Respir Crit Care Med 52:1028–1033
Orozco-Levi M, Torres A, Ferrer M, Piera C, el-Ebiary M, de la Bellacasa JP, Rodriguez-Roisin R (1995) Semirecumbent position protects from pulmonary aspiration but not completely from gastroesophageal reflux in mechanically ventilated patients. Am J Respir Crit Care Med 152:1387–1390
McMullin JP, Cook DJ, Meade MO, Weaver BR, Letelier LM, Kahmamoui K, Higgins DA, Guyatt GH (2002) Clinical estimate of trunk position among mechanically ventilated patients. Intensive Care Med 28:304–309
Berra L, De Marchi L, Panigada M, Lewandowki R, Appleton J, Costello K, Villa F, Mahar R, Kolobow T (2003) Effects of continuous aspiration of subglottic secretions on tracheal integrity and bacterial colonization of the respiratory tract and role of tracheal tube orientation (abstract). International Conference of the American Thoracic Society, Seattle
Miller RL, Cole RP (1996) Association between reduced cuff leak volume and postextubation stridor. Chest 110:1035–1040
Darmon JY, Rauss A, Dreyfuss D, Bleichner G, Elkharrat D, Schlemmer B, Tenaillon A, Brun-Buisson C, Huet Y (1992) Evaluation of risk factors for laryngeal edema after tracheal extubation in adults and its prevention by dexamethasone. Anesthesiology 77:245–251
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Girou, E., Buu-Hoi, A., Stephan, F. et al. Airway colonisation in long-term mechanically ventilated patients. Intensive Care Med 30, 225–233 (2004). https://doi.org/10.1007/s00134-003-2077-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-003-2077-4