Abstract
Aims/hypothesis
Hydrogen sulphide is a recently identified endogenous endothelium-dependent vasodilator. Animal models of diabetes have shown that low plasma H2S levels are associated with marked endothelial dysfunction and insulin resistance. However, human studies on H2S and vascular function in health and disease are lacking.
Methods
Plasma was obtained from male patients with type 2 diabetes (n = 11), overweight (n = 16) and lean (n = 11) volunteers. H2S levels were determined by zinc trap spectrophotometry. Anthropometric measurements (BMI/waist:hip ratio), lipid profile, systemic blood pressure, biochemical indices of diabetes (fasting glucose, insulin sensitivity, Hb1Ac) and microvascular function (minimum vascular resistance) were determined.
Results
Median plasma H2S levels (25th, 75th percentiles) in age-matched lean, overweight and type 2 diabetes individuals were 38.9 (29.7, 45.1) µmol/l, 22.0 (18.6, 26.7) µmol/l and 10.5 (4.8, 22.0) µmol/l, respectively. Median plasma H2S levels were significantly lower in patients with type 2 diabetes compared with lean (p = 0.001, Mann–Whitney) and overweight participants (p = 0.008). Median plasma H2S levels in overweight participants were significantly lower than in lean controls (p = 0.003). Waist circumference was an independent predictor of plasma H2S (R 2 = 0.423, standardised beta: −0.650, p < 0.001). This relationship was independent of diabetes, which only contributed a further 5% to the model (R 2 = 0.477). Waist circumference or other measures of adiposity (waist:hip ratio/BMI) remained independent predictors of plasma H2S after adjustment for systolic blood pressure, microvascular function, insulin sensitivity, glycaemic control and lipid profile.
Conclusions/interpretation
Plasma H2S levels are reduced in overweight participants and patients with type 2 diabetes. Increasing adiposity is a major determinant of plasma H2S levels.
Similar content being viewed by others
Introduction
Hydrogen sulphide is endogenously produced in the mammalian vasculature from the amino acids cysteine and homocysteine by the pyridoxal-5′-phosphate-dependent enzyme cystathionine-γ-lyase (CSE; EC 4.4.1.1) (reviewed in Whiteman and Moore [1]). Vascular H2S acts as an endothelium- and KATP-channel-dependent vasodilator [1] and plasma and serum H2S levels in rodents and healthy humans are reported to be in the range 40–80 µmol/l [1]. Higher levels of H2S have been observed in animal models of endotoxic and haemorrhagic shock, in which pharmacological inhibition of CSE using d,l-propargylgycline significantly increased blood pressure and survival (reviewed in Li et al. [2]). Conversely, lower H2S levels were reported in animal models of hypertension, in which the administration of H2S ‘donors’ decreased blood pressure [1]. These observations are consistent with the role of H2S as an endogenous vasodilator.
Recently, a role for H2S in the aetiology of diabetes has been suggested. Pancreatic synthesis of H2S is markedly elevated in the streptozotocin (STZ) rat [3], in which biphasic effects on beta cells have been observed; at low concentrations, H2S inhibited insulin release through KATP-dependent/Ca2+-independent mechanisms [4], whereas higher levels induced beta cell death through endoplasmic-reticular-stress-dependent pathways [5]. However, plasma H2S levels were lower after STZ treatment [3]. Similarly, in the NOD mouse, plasma levels of H2S and the responsiveness of vascular tissue to endothelium-dependent vasodilators, such as acetylcholine, declined and aortic synthesis of H2S were also progressively reduced as diabetic pathology increased [6].
Since there is increased risk of hypertension and cardiovascular disease and loss of vascular responsiveness to endogenous vasodilators in individuals with type 2 diabetes mellitus and obesity, we investigated whether there would also be a loss of vasodilatory H2S in type 2 diabetes and obesity.
Methods
Participants
Participants were recruited from advertisements in the local community. Individuals were excluded from the study if they had suffered a stroke or myocardial infarction, or had uncontrolled hypertension (>160/90 mmHg). Participants with type 2 diabetes were also excluded if they were treated with insulin. Additional exclusion criteria are listed in the Electronic Supplementary Material (ESM). Three study groups were recruited: (1) lean men (BMI < 25.0 kg/m2) (n = 11); (2) age-matched overweight men (BMI > 25.0 kg/m2) (n = 16); and (3) age-matched men with type 2 diabetes who were BMI matched (to within ±2 kg/m2) to the overweight non-diabetic men (n = 11). Participants’ characteristics are shown in Table 1. All assessments were performed in a temperature-controlled laboratory (22.0 ± 0.5°C) with the participants having fasted from 22:00 hours the previous evening and having taken no medication on the morning (09:00 hours) of the tests. All patients provided written informed consent. The study was approved by the Devon and Torbay Ethics Committee and was performed in accordance with principles of the Declaration of Helsinki.
Measurement of plasma H2S
Peripheral blood samples (10 ml; EDTA anti-coagulated) were collected as described previously [1, 3, 4, 6]. H2S levels were determined in triplicate as described previously [1–6] and concentrations calculated against a calibration curve of sodium sulphide (1.06–100 µmol/l; Sigma-Aldrich, MO, USA). Briefly, 250 μl zinc acetate (1% wt/vol. in water) was injected into 200 μl plasma in tightly sealed Eppendorf vials followed by injection of 133 μl N,N-dimethyl-p-phenylenediamine sulphate (20 mmol/l in 7.2 mol/l HCl; Sigma-Aldrich) and 133 μl FeCl3 (30 mmol/l in 1.2 mol/l HCl; Sigma-Aldrich) [1, 3, 4, 6]. After incubation in the dark for 30 min, samples were centrifuged at 5,000 g for 10 min and the absorbance of the supernatant fraction at 670 nm determined. The intra-assay coefficient of variation was 0.1–3.76% over the concentration range studied (n = 12). No significant interference was observed in the presence of physiological concentrations of sulphite (SO 2−3 ), sulphate (SO 2−4 ), thiosulphate (S2O 2−3 ), reduced glutathione, oxidised glutathione, cysteine, cystine, homocysteine, homocystine, cystathionine, methionine, nitrite (NO −2 ) or nitrate (NO −3 ), (p = NS, Kruskal–Wallis; n = 4). At physiological pH, H2S (pK a 7.04) dissociates to the hydrosulphide anion (HS−) and the sulphide anion (S2−) [1]. Therefore, we use the term H2S to refer to the sum of these species (H2S, HS− and S2−) present at physiological pH [1, 3, 4].
Systemic blood pressure
Supine blood pressure was measured from the left arm using a semi-automatic blood pressure recorder (Critikon Dinamap, Deltona, FL, USA). Five measurements were obtained at 1 min intervals and the mean of the final three readings was taken to be the representative blood pressure.
Microvascular assessment
Maximum hyperaemia was assessed by heating a small area of skin to 42–44°C [7], which induces maximum hyperaemia. This was achieved by attaching a small brass heater (area 0.76 cm2) to the dorsum of the foot for 30 min. The resultant maximum hyperaemic response was assessed by single-point laser Doppler fluximetry (LDF; Perflux Pf2: Perimed, Järfälla Sweden), eight equally spaced measurements were made within the heated area and the mean used to represent maximum hyperaemia, arbitrarily expressed as volts. Day-to-day intra-individual variation with this technique is 6.6% (mean ± standard deviation: 1.81 ± 0.12 V) in one participant assessed over five separate occasions. Minimum vascular resistance (MVR) of the skin microcirculation was calculated by dividing mean arterial pressure (MAP) by maximum hyperaemia (MVR = MAP/MH, mmHg/V) [7].
Insulin sensitivity assessments
Central insulin sensitivity was calculated by HOMA insulin sensitivity, based on fasting insulin and glucose levels [8]. Peripheral insulin sensitivity was assessed using a 15 min continuous insulin tolerance test (ITT) [7]. A bolus of 0.1 U kg−1 of insulin (Human Actrapid; Novo Nordisk Pharmaceuticals, Crawley, UK) was administered into a vein at the site of the anticubital fossa. Blood samples for the determination of blood glucose were taken each minute until the blood glucose level reached 3 mmol/l or 15 min duration was reached [7]. The glucose samples were measured in duplicate (YSI2300 Stat Plus; Yellowsprings Instruments, Yellowsprings, OH, USA). The slope of the blood glucose curve was used to represent insulin sensitivity [7].
Biochemical variables
All blood samples were obtained after assessment of microcirculatory function. HbA1c (normal range 4.0–6.0%) was determined using an in-house high performance liquid chromatography method (Hewlett Packard 1050 HPLC) [7]. Fasting glucose was determined using a glucose oxidase method (GOD-PAP; Roche Modular analyser, Roche Diagnostics, Lewes, UK) [7]. Triacylglycerol, lipids and cholesterol were determined using a colorimetric assay (using a Vitros Analyser; Johnson & Johnson Clinical Diagnosis, Amersham, UK) [7]. An electrochemiluminescence assay was used for the determination of fasting plasma insulin (0.05% cross-reactivity with human proinsulin) (Cobas; Roche, Basel, Switzerland) [7].
Statistical analysis
Statistical analysis was performed by the Statistical Package for Social Sciences (SPSS) version 15.0 (Chicago, IL, USA). The Mann–Whitney test was used for between-group analyses. To enable the examination of associations between H2S levels and diabetes and obesity, data from the three participant groups were merged (n = 38) to generate a continuum of data. An adiposity measure (waist circumference, waist:hip ratio or BMI) and diabetes status were initially entered into a forced regression model. To determine whether the relationship between plasma H2S with obesity and diabetes status was influenced by their related milieu, potential confounders—such as systolic blood pressure, fasting glucose, HbA1c, minimum vascular resistance, insulin sensitivity as assessed by both HOMA and insulin tolerance test—were each entered into separate regression models. Data were checked to ensure the assumptions required for regression analysis were fulfilled. This study was powered to detect a between-individual difference of 1.4 standard deviations, and a large effect size (f 2 = 0.420) with three predictors in the linear regression model at the 5% level with 90% power. p values less than 0.05 were considered significant.
Results
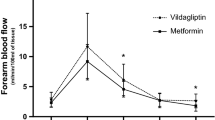
Participant demographics are shown in Table 1. Median plasma H2S levels (25th, 75th percentiles) in lean controls, overweight volunteers and men with type 2 diabetes were 38.9 (29.7, 45.1) µmol/l, 22.0 (18.6, 26.7) µmol/l and 10.5 (4.8, 22.0) µmol/l, respectively (Fig. 1). Median plasma H2S levels were significantly lower in patients with type 2 diabetes compared with age-matched controls (p = 0.001) and overweight men (p = 0.008), presumably because of the increased adiposity of the type 2 diabetes group. Median plasma H2S levels in overweight volunteers were also significantly lower than in lean age-matched controls (p = 0.003). In the univariate analysis, plasma H2S was negatively correlated with systolic (r = −0.580, p < 0.001) and diastolic (r = −0.527, p < 0.001) blood pressures, glycaemic control (fasting glucose, r = −0.494, p = 0.001; Hb1Ac, r = −0.423, p = 0.006) and insulin sensitivity (peripheral insulin [ITT], r = −0.497, p = 0.004; central insulin [HOMA], r = 0.566, p < 0.001). Microvascular function tests further showed significant associations with plasma H2S (maximum hyperaemia, r = 0.402, p = 0.008; minimum vascular resistance, r = −0.436, p = 0.004). However, the strongest correlations were observed with measurements of adiposity i.e. waist circumference (r = −0.650, p < 0.001), waist:hip ratio (r = −0.657, p < 0.001), BMI (r = −0.609, p < 0.001) and, to a lesser extent, hip circumference (r = −0.358, p = 0.017). Regression analysis suggested that adiposity, as assessed by waist circumference, but not diabetes status was a significant independent predictor of plasma H2S levels (waist circumference: standardised beta: −0.543, p = 0.001; diabetes status: standardised beta: −0.257, p = 0.077). The observed independent relationship between waist circumference and plasma H2S remained after adjusting for the potential confounders: systolic blood pressure, minimum vascular resistance, age, central insulin sensitivity (HOMA) and total cholesterol:HDL ratio (standardised beta range of −0.432 to −0.541, p value range 0.01–0.001; ESM Table 1). Similar trends were observed between plasma H2S and other measures of adiposity (i.e. waist:hip ratio and BMI; ESM Tables 2 and 3, respectively). Waist:hip ratio, but not BMI or waist circumference, was an independent predictor of plasma H2S levels when adjusting for peripheral insulin sensitivity (waist:hip ratio: −0.407, p = 0.029; waist circumference: −0.283, p = 0.109; BMI: −0.183, p = 0.329), suggesting that the relationship between adiposity and plasma H2S may be related to peripheral insulin sensitivity. However, diabetes status was not a significant independent predictor of plasma H2S in any of these models in this study.
Plasma H2S levels in lean healthy and overweight volunteers and patients with type 2 diabetes mellitus. Plasma (EDTA) was collected from participants and each sample analysed in triplicate for H2S as described in the Methods. Data are expressed as median (25th and 75th percentiles). All samples were age matched. Overweight volunteers were matched by BMI to type 2 diabetic patients. The Mann–Whitney test was used to determine differences between sample groups with significance set at p < 0.05. Lean controls vs overweight (p = 0.003), lean controls vs type 2 diabetic patients (p = 0.001), overweight vs type 2 diabetic patients (p = 0.008). Outlying data points are shown by crosses
Discussion
It is well established that diabetes is associated with the clustering of central obesity, dyslipidaemia, raised blood pressure, hyperglycaemia and increased risk of cardiovascular disease [9]. However, the precise molecular mechanisms underpinning these clinical associations are currently not known. H2S is emerging as important vasodilatory intermediate, inducing endothelium-dependent and KATP-channel-dependent vasorelaxation in vitro and in vivo. Our current observations that plasma H2S levels negatively correlated with systolic and diastolic blood pressure, microvascular dysfunction, glycaemic control and insulin sensitivity are the first in man and are consistent with the observations in animal models of diabetes and hypertension [1, 3, 6].
A potential role for CSE-derived H2S in adipose fat metabolism has also been proposed in rats [10]. In our study, the major determinant of plasma H2S levels was adiposity. This relationship was not accounted for by diabetes status, glycaemic control, blood pressure, microvascular function, lipids or central insulin sensitivity. However, when adjusting for peripheral insulin sensitivity, the independent relationships of plasma H2S levels with BMI and waist circumference—but not waist:hip ratio—were lost, suggesting that peripheral insulin sensitivity may be contributing to the relationship between adiposity and plasma H2S.
A limitation of the current study is the potential for a type 2 error. However, the fact that H2S was consistently associated with adiposity as assessed by BMI, waist circumference and waist:hip ratio, endorses the proposal that an increase in adiposity is associated with a reduction in plasma levels of H2S. However, further longitudinal studies with increased sample sizes are required to substantiate the precise relationship between plasma levels of H2S and diabetes.
In summary, our study has shown that adiposity is a major determinant of plasma levels of H2S. The loss of the vasodilatory gas H2S could represent a novel mechanism for mediating cardiovascular complications in obesity and type 2 diabetes. Whether this loss occurs because of reduced H2S synthesis, enhanced enzymatic removal or increased consumption by oxidants known to be elevated in the diabetic milieu requires further attention.
Abbreviations
- CSE:
-
Cystathionine-γ-lyase
- ITT:
-
Insulin tolerance test
- KATP channels:
-
ATP-dependent potassium channels
- MVR:
-
Minimum vascular resistance
- STZ:
-
Streptozotocin
References
Whiteman M, Moore PK (2009) Hydrogen sulfide and the vasculature: a novel vasculoprotective entity and regulator of nitric oxide bioavailability? J Cell Mol Med 13:488–507
Li L, Hsu A, Moore PK (2009) Actions and interactions of nitric oxide, carbon monoxide and hydrogen sulphide in the cardiovascular system and in inflammation—a tale of three gases! Pharmacol Ther 123:386–400
Yusuf M, Huat BTK, Hsu A, Whiteman M, Bhatia M, Moore PK (2005) Streptozotocin-induced diabetes in the rat is associated with enhanced tissue hydrogen sulfide biosynthesis. Biochem Biophys Res Commun 333:1146–1152
Ali MY, Whiteman M, Low CM, Moore PK (2007) Hydrogen sulphide reduces insulin secretion from HIT-T15 cells by a KATP channel-dependent pathway. J Endocrinol 195:105–112
Yang G, Yang W, Wu L, Wang R (2007) H2S, endoplasmic reticulum stress, and apoptosis of insulin-secreting beta cells. J Biol Chem 292:16567–16576
Brancoleone V, Roviezzo F, Velleco V, De Gruttola L, Bucci M, Cirino G (2008) Biosynthesis of H2S is impaired in non-obese diabetic (NOD) mice. Br J Pharmacol 155:673–680
Middlebrooke AR, Elston LM, Macleod KM et al (2006) Six months of aerobic exercise does not improve microvascular function in type 2 diabetes mellitus. Diabetologia 49:2263–2271
Matthew DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta cell function from fasting glucose and insulin concentrations in man. Diabetologia 28:214–419
Hajer GR, van Haeften TW, Visseren FL (2008) Adipose tissue dysfunction in obesity, diabetes, and vascular diseases. Eur Heart J 29:2959–2971
Feng X, Chen Y, Zhao J, Tang C, Jiang Z, Geng B (2009) Hydrogen sulfide from adipose tissue is a novel insulin resistance regulator. Biochem Biophys Res Commun 380:153–159
Acknowledgements
This work was supported by the Peninsula National Institute for Health Research (NIHR) Clinical Research Facility and funded by the Northcott Devon Medical Research Foundation, the Diabetes Research and Education Centre Trust (DIRECT) and Diabetes UK. The opinions expressed by the authors of this manuscript are not necessarily those of NIHR, the National Health Service or the Department of Health (England and Wales).
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Whiteman, M., Gooding, K.M., Whatmore, J.L. et al. Adiposity is a major determinant of plasma levels of the novel vasodilator hydrogen sulphide. Diabetologia 53, 1722–1726 (2010). https://doi.org/10.1007/s00125-010-1761-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-010-1761-5